NEJM:他汀不能预防心脏手术后房颤(STICS研究)
2016-05-05 MedSci MedSci原创
5月5日,由国家心血管病中心阜外医院心血管外科郑哲研究团队与英国牛津大学合作开展的关于心脏手术围手术期使用他汀药物治疗房颤的大规模随机对照双盲临床试验——STICS研究结果发表于国际医学领域的顶级权威期刊《新英格兰医学杂志》STICS ClinicalTrials.gov number, NCT01573143.)。 房颤是最为常见的心律失常性疾病,有关资料显示我国房颤患者人数达8
5月5日,由国家心血管病中心阜外医院心血管外科郑哲研究团队与英国牛津大学合作开展的关于心脏手术围手术期使用他汀药物治疗房颤的大规模随机对照双盲临床试验——STICS研究结果发表于国际医学领域的顶级权威期刊《新英格兰医学杂志》(STICS ClinicalTrials.gov number, NCT01573143.)。
房颤是最为常见的心律失常性疾病,有关资料显示我国房颤患者人数达800万,房颤可使患者脑卒中发生率增加5倍,心衰发生率增加3倍。术后房颤是心脏手术术后最常见的并发症之一,发生率高达35%至50%。其所造成的患者血流动力学不稳定,能够显著增加脑卒中、心血管死亡的发生风险,同时会对患者康复造成不利影响,延长住院时间并增加医疗费用。
既往研究显示,高胆固醇水平也是影响心血管疾病发生发展的重要危险因素。持续服用他汀药物降低低密度脂蛋白胆固醇(LDL-C)是预防心血管事件的重要举措。阜外医院前期开展的心脏预防研究(HPS)结果显示,应用辛伐他汀降低LDL-C对血管合并症和死亡有积极的预防作用。另一方面,与心脏手术和体外循环相关的氧化应激和炎症反应是术后房颤发生的罪魁祸首。心房NADPH氧化酶2(NOX2)活性是预测术后新发房颤的独立因子,心房NOX2活性越强,房颤的发生率也越高。研究表明,他汀不仅可以通过竞争性抑制HMG-CoA还原酶而起到降低LDL-C的作用,还可抑制NOX2活性,其抗炎、抗氧化应激的作用也逐步为基础和临床研究所证实。
已有的小规模临床研究显示,他汀类药物能够降低心脏术后房颤的发生,减少心肌损伤,改善左心室功能,保护肾功能,缩短重症监护和住院时间。“目前欧洲冠脉再血管化治疗指南(2014)推荐搭桥手术后应接受他汀治疗维持LDL-C<70mg/dl,美国冠状动脉旁路移植指南(2011)及冠状动脉旁路移植二级预防指南(2015)亦强烈建议所有行搭桥手术的患者围术期接受他汀治疗,除非患者有明确用药禁忌。”STICS研究主要负责人,阜外医院郑哲教授提到,“尽管他汀药物在心脏手术,特别是冠状动脉旁路移植术围术期的应用已成为业内共识,其降低心脏术后并发症的效益仍众说纷纭,且药物作用机制也尚未完全阐明”。
STICS研究以心脏手术领域他汀药物治疗的现存争议为核心,在研究设计之初就备受业内关注。研究的英国方合作者,牛津大学的Barbara Casadei教授是国际知名的房颤疾病发生机制和临床治疗研究领域专家。阜外医院郑哲教授领衔的心血管外科研究团队凭借丰富的国际合作临床研究开展经验,从患者入选、治疗干预、样本采集等各环节严密把关,保障该研究的顺利进行。研究曾入选2014年8月在巴塞罗那召开的欧洲心脏病学学会(ESC)年会六大亮点研究,并被特邀在2015年中国心脏大会开幕式上作了主题报告。
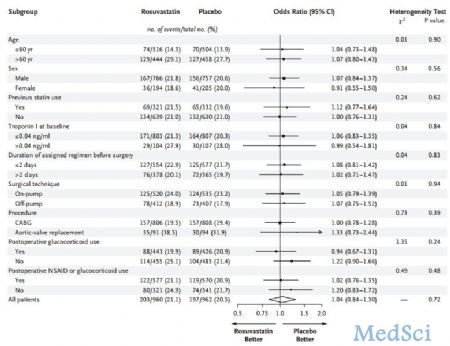
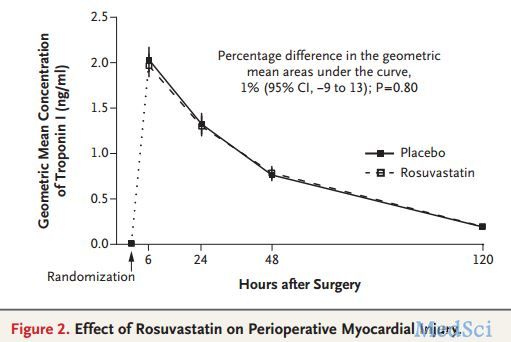
STICS研究是严格按照国际标准设计实施的随机、双盲、安慰剂对照临床试验,从设计到完成历时超过5年。研究共纳入阜外医院1922例窦性心律无房颤史且拟择期接受心脏手术的患者。受试者均在术前8天开始服用瑞舒伐他汀(20 mg/d),在术后第5天停药。主要研究终点为术后房颤发生率(Holter ECG监测)和心肌损伤(术后第6,24,48,120小时肌钙蛋白水平)。次要研究终点为术后重症监护时间、心脑血管事件、左心室射血分数、肾功能、LDL-C以及NT-proBNP水平。研究发现,与安慰剂相比,瑞舒伐他汀确实可以显著降低LDL-C水平,但并没有降低术后肌钙蛋白水平(102 ng-hr/mL versus 100 ng-hr/mL, P=0.80)和房颤的发生率(21% vs 20%,P=0.72),也没有缩短住院时间,相反还会增加肾功能损伤(24.7% vs 19.3%,P=0.0047)。
郑哲教授认为,尽管研究结论可能受到研究人群、样本量和他汀种类等因素的影响,但研究的整体结论和亚组分析结果对临床现有认识和实践仍具有重要的提示作用。“我们必须意识到,一方面,现有的研究证据难以全面支持临床指南中关于他汀药物在心脏手术围术期的应用规范,更新后的欧洲再血管化治疗指南确实对他汀治疗策略有所细化,但依旧面临客观证据不足的窘境;另一方面,心脏手术的不同类型、患者个体的差异等因素应对他汀药物的个性化使用起到指导作用,以实现治疗效益的准确化和最大化。”
据悉,STICS研究是国家心血管病中心阜外医院获准设立国家心血管疾病临床医学研究中心后完成的又一项高水平、标准化国际合作临床研究,同时也是中国学者在国际心血管领域取得的又一杰出成果。该研究是全球范围内迄今为止最大规模评价他汀药物在心脏手术围术期应用有效性的临床研究,采用术后连续、客观监测的房颤和心肌损伤为研究终点,研究结论打破了国际上以往他汀治疗降低心脏术后并发症的传统观点,为现行的临床指南和诊疗常规提出了挑战并提供了全新的参考和借鉴,这必将为他汀药物围手术期治疗的进一步规范和后续研究的开展起到积极而重要的推动作用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#术后房颤#
60
要是用的再便宜点就好了
144
用不起啊
161
积分积分
154
好难搞到
160
学习了,很好的
140
这个app真好
92
临床和科研的完美结合
44
好文章,值得深究学习
157
好文章,值得深究学习
97