多项肿瘤标志物升高竟是因为它
2021-12-11 侯兵兵 齐文峰 李小乐 “检验医学”公众号
近年来,很多体检机构逐渐将肿瘤标志物加入到了体检项目中用于肿瘤筛查。本文遇到一例健康受检者多项肿瘤标志物异常而其他检查结果未见异常的案例,现报道如下。
前言
临床上血清中肿瘤标志物的检测一般用于肿瘤的协助诊断、鉴别诊断、治疗后评估和复发监测等。近年来,很多体检机构逐渐将肿瘤标志物加入到了体检项目中用于肿瘤筛查。本文遇到一例健康受检者多项肿瘤标志物异常而其他检查结果未见异常的案例,现报道如下。
案例经过
患者:女,32岁,于2021年8月27日在我院进行单位年度健康体检,检验科在对其肿瘤标志物监测时发现该被检者多项肿瘤标志物均升高。肿瘤标志物检测结果如图1:
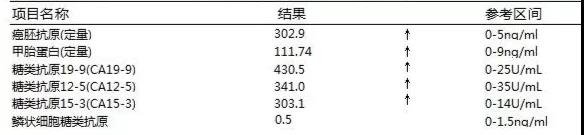
图1
由图1可知:该患者肿瘤标志物中除SCC外CEA、AFP、CA199、CA125、CA153均异常。由于该患者为健康体检人员,极少出现多项肿瘤标记物同时升高的现象,于是我们对其体检套餐中其他检测和检查结果(B超、CT、X线等)进行查询,发现该患者其他体检项目结果均未见异常。
为了进一步确定肿瘤标志物检测结果的可靠性,按着我实验室制定的“实验室异常结果处理流程图”(如图2)进行以下处理。
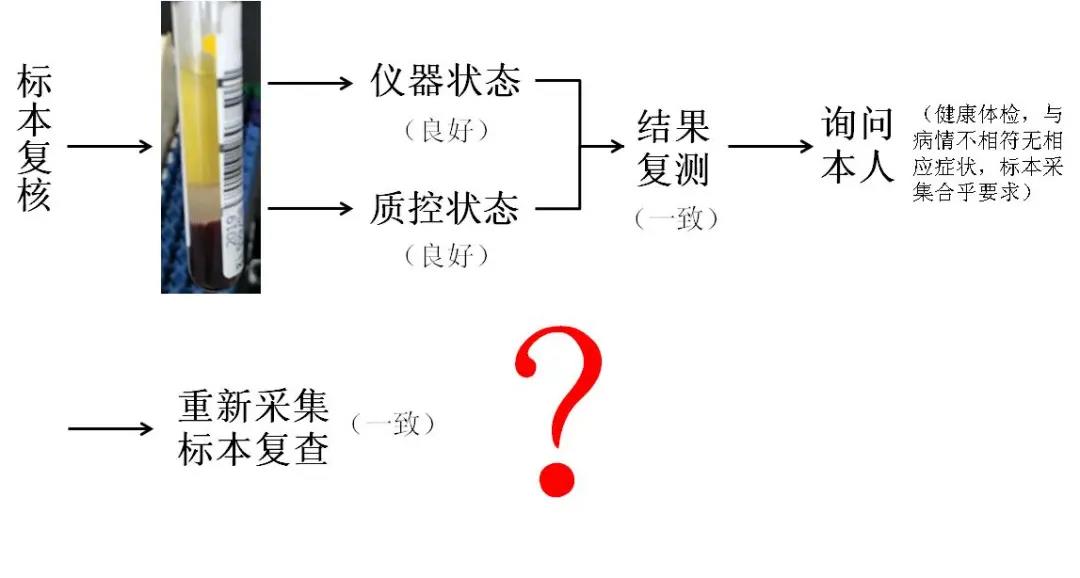
图2
具体处理结果如下:
(1)标本复核:标本状态良好,未见有脂血、溶血、纤维丝(块)等异常;
(2)仪器状态:仪器状态良好未见仪器异常报警信息。
(3)质控状态:质控状态良好,未触及我实验室“1-3S,2-2S”质控规则。
(4)结果复测:对原始标本在另一台同型号化学发光分析仪上进行肿瘤标志物复测,升高的几项肿瘤标记物仍升高,结果一致。
(5)询问体检科主检医生和受检者本人:健康体检,结果均正常,身体未出现明显异常症状。
(6)重新采集标本复检:对患者血液标本进行重新采集,肿瘤标志物复测,结果仍异常升高!
经上述处理后我们可知,该受检者除肿瘤标志物外其他各项检查均未见异常!但是,到底是什么原因导致该受检者多项肿瘤标志物结果升高呢?
此时我们注意到,该受检者肿瘤标记物中只有SCC没有升高,而这几项肿瘤标志物中SCC与其他升高的肿瘤标志物并不是在同一厂家仪器上检测的。于是,我们将该受检者标本放到与SCC相同检测仪器平台上进行检测,结果发现原来检测异常的肿瘤标志物均正常了。
案例分析
从上述过程我们可初步判断,该受检者多项肿瘤标志物异常原因可能是标本内存在干扰物质导致结果异常。为进一步确定是否存在检测干扰物,我们将该标本送至厂家实验室进行常见干扰物质检测,结果为该受检者体内存在鼠源性异嗜性抗体。
我们查阅CEA、AFP、CA199、CA125、CA153这几项肿瘤标志物的试剂说明书发现,均采用的双位点酶免法(“夹心法”)原理,试剂内抗体均为小鼠单克隆抗体。因此,我们可确定本案例中CEA、AFP、CA199、CA125、CA153多项肿瘤标志物检测结果(图1)为假性升高。
由于抗原抗体反应比较复杂,容易受到体内某些抗体干扰。当我们在工作中遇到此类情况怀疑存在干扰物质时,可采用梯度稀释的方法或者更换不同的厂家仪器平台进行确认,也可在厂家帮助下对标本进行“阻断实验”来最终确定是否存在干扰物。
小结
异嗜性抗体为人体内源性抗体,可与动物免疫球蛋白的的Fc或F(ab,)2段结合,从而影响抗原抗体反应。有研究表明,双抗体夹心法受异嗜性抗体干扰最严重(尤其是使用鼠源性单克隆抗体)。一般人群中约3-15%的人体内含有异嗜性抗体,多为接触动物、动物制品或接种动物血清类疫苗后产生的。在日常工作中异嗜性抗体导致肿瘤标志物假性升高的情况时有发生,当我们遇到类似情况时一定要结合患者临床实际情况然后进行报告审核签发,必要时可更换检测平台进行检测或向试剂厂家进行求助。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#标志物#
67
学习了,受益匪浅
82
收到
99
阅国内外无数文献,经过反复推敲和打磨,改版数十次后精心汇编而成
107
谢谢分享!
103