NEJM:中等手术风险的主动脉瓣狭窄患者是选择手术换瓣还是TAVR?
2017-03-19 xing.T MedSci原创
由此可见,TAVR是手术风险中等的主动脉瓣狭窄患者一种非劣效性替代方法。
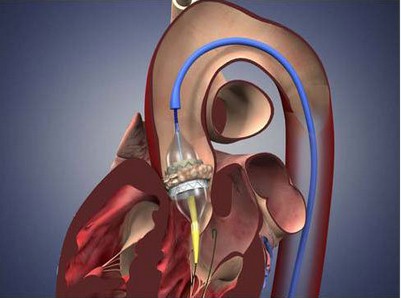
对于高手术风险的严重主动脉瓣狭窄的患者,尽管经导管主动脉瓣置换术(TAVR)是一种可接受的手术替代方法,但是对于手术风险中等的主动脉瓣狭窄患者比较结果尚不明确。近日,顶级医学期刊NEJM上针对这一问题发表了一篇研究文章。
研究人员评估了比较TAVR和主动脉瓣置换手术的随机试验中具有中等风险的严重、症状性主动脉狭窄患者的临床结局。该研究的主要终点是患者接受主动脉瓣置换后24个月内任何原因的死亡或致残性卒中的复合。研究人员采用贝叶斯分析方法(0.07的优势)评价TAVR的非劣效性,与外科瓣膜置换术相比较。
在87个中心中,共有1746例患者参与随机化分组。这些患者中,1660接受了TAVR或外科手术。患者平均年龄为79.8岁±6.2岁,所有参与者均为外科手术中等风险(胸外科医师预测死亡风险为4.5±1.6%)。在24个月时,主要终点的估计发生率在TAVR组为12.6%,在对照组为14%(差异的95%可信区间[贝叶斯分析]为-5.2至2.3%;非劣效性的后验概率>0.999)。手术与较高的急性肾损伤、房颤和输血需求相关,而TAVR发生残留主动脉瓣关闭不全和心脏起搏器植入术的需求率较高。TAVR比手术会导致更低的平均压力梯度和较大的主动脉瓣面积。在24个月,两组患者瓣膜结构性恶化都没有发生。
由此可见,TAVR是手术风险中等的主动脉瓣狭窄患者一种非劣效性替代方法。
原始出处:
Michael J. Reardon, et al. Surgical or Transcatheter Aortic-Valve Replacement in intermediate-Risk Patients. N Engl J Med 2017; http://www.nejm.org/doi/full/10.1056/NEJMoa1700456
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#AVR#
82
#主动脉瓣#
81
#主动脉#
77
#手术风险#
98