JACC:TAVR过程中,比伐卢定并不优于肝素的效果
2015-12-22 MedSci MedSci原创
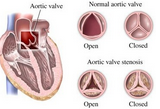
抗凝治疗是经导管主动脉瓣置换术(TAVR)的必需程序。虽然一个最佳方案尚未确定,但主要用肝素。直接凝血酶抑制比伐卢定可能是在此过程中用于抗血凝剂一种有效的替代肝素药物。 本研究的目的是确定是否比伐卢定可以替代肝素作为接受TAVR的患者的抗凝血剂。共有802例主动脉瓣狭窄患者被随机分配接受经股TAVR比伐卢定 vs 肝素。2个主要终点是48小时内或出院前严重出血事件(以先发生为准)和30天
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#比伐卢定#
67
#JACC#
59
#AVR#
58
好文章!
131
嗯,
127
#ACC#
76
收藏
154
不错的东东
132