SCI REP:非酒精性脂肪肝与冠状动脉钙化有何关系?
2017-08-30 xing.T MedSci原创
由此可见,该研究的发现进一步证实了NAFLD与CAC之间存在的关联,特别是在亚洲人群中。
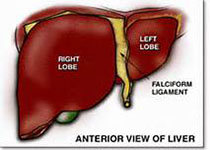
非酒精性脂肪肝(NAFLD)已成为一个新兴的健康问题,在一般人群中发病率很高。近日,Scientific reports 杂志上发表了一篇研究文章,在这个横断面研究中,研究人员通过分析中国北方城市居民探讨了NAFLD与冠状动脉钙化(CAC)之间的关联。
该研究共有2345名年龄≥40岁(1035名男性和1310名女性)选自于唐山市鸡东社区的参与者。研究人员通过肝脏超声检查来诊断NAFLD。64层螺旋CT扫描被用于测定冠状动脉钙化积分(CACS),CACS>0定义为存在CAC。冠状动脉粥样硬化性心脏病(CHD)的风险水平根据在临床实践中常用的CACS4种阈值来进行分级(0、10、100和400Agatston单位)。
研究人员发现NAFLD与CAC显著相关(粗略OR为1.631,95%CI为1.295-2.053,调整后的OR为1.348,95%CI为1.030-1.765)。研究人员也观察到了非酒精性脂肪性肝病与冠心病风险增加之间存在相关性(粗略OR为1.639,95%CI为1.303-2.063;调整后的OR为1.359,95%CI为1.043-1.770)。在女性中,非酒精性脂肪肝与CAC或冠心病风险增加之间具有显著性差异,但在男性中并无显著性差异。
由此可见,该研究的发现进一步证实了NAFLD与CAC之间存在的关联,特别是在亚洲人群中。
原始出处:
Rina Wu,et al. Nonalcoholic Fatty Liver Disease and Coronary Artery Calcification in a Northern Chinese Population: a Cross Sectional Study.Scientific reports. 2017. https://www.nature.com/articles/s41598-017-09851-5
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#非酒精性#
70
#酒精性#
74
#冠状动脉钙#
73
#酒精性脂肪肝#
58
#动脉钙化#
104
未来的发展前景广阔
107
好文.值得点赞!认真学习了.把经验应用于实践.为患者解除病痛.
117
学习了
101
#冠状动脉钙化#
73
学习了谢谢分享
121