JAHA:Fontan手术后肝癌的发病率、预测指标和死亡率
2021-02-06 MedSci原创 MedSci原创
在Fontan手术30年后,LC的发生率迅速增加,肝纤维化指标和AFP可作为新发LC的预测指标。应严格监控这些LC预测标记物,以尽早发现LC和改善患者预后。
Fontan手术后,肝癌(LC)是严重的晚期并发症。但是,其发病率、预测因素和预后仍然未知。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员旨在明确这些患者的临床特征。研究人员评估了2005年至2019年期间接受过Fontan手术的339例患者的肝功能。
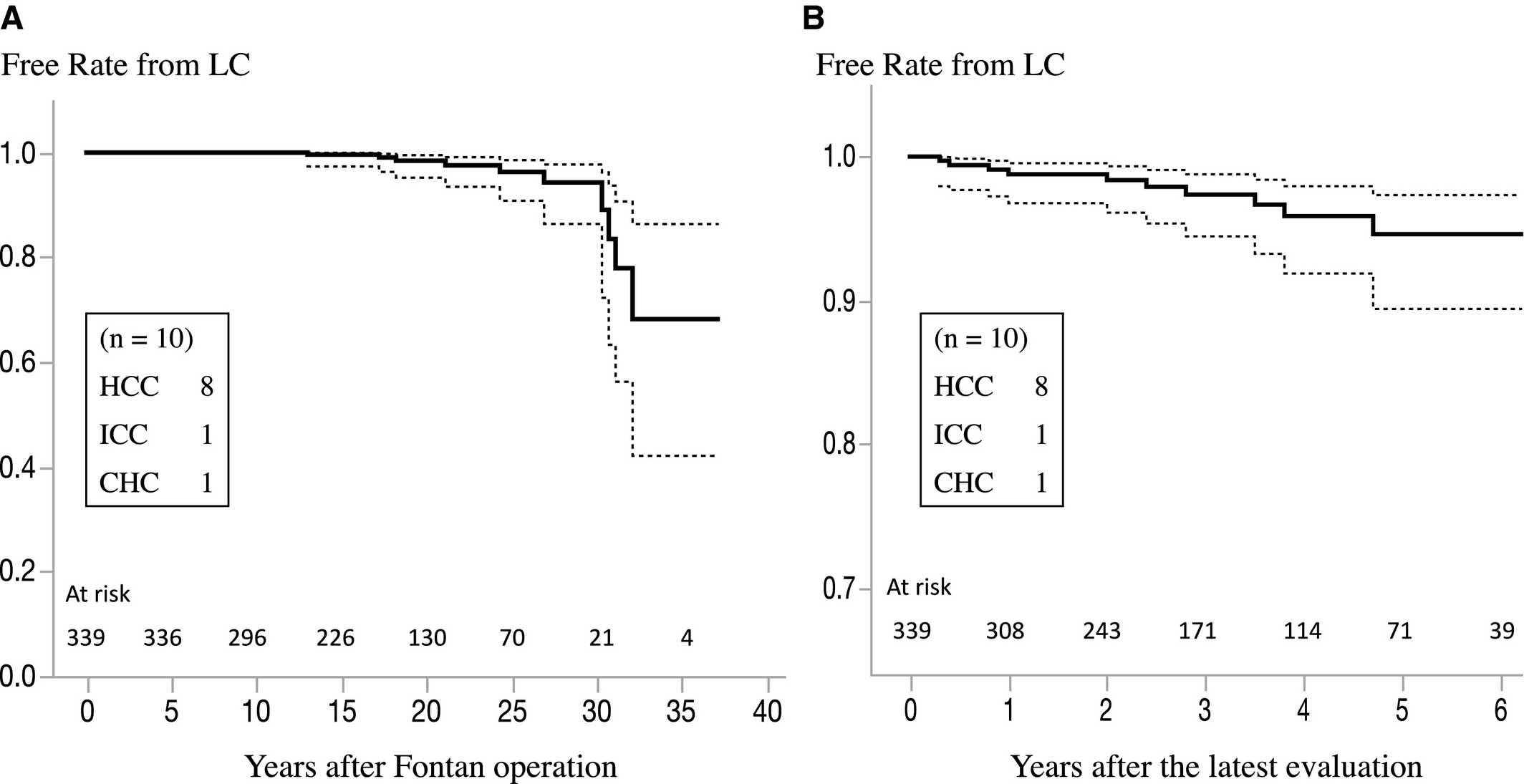
在中位时间为2.9年的随访期间,有10例患者在组织学上诊断为LC(范围:0.3-13.8;中位年龄为29.9岁[范围为14.4-41.5岁];Fontan手术后随访年龄的总体中位数为25.6岁[范围:13-32.1岁]),LC年发病率为0.89%。在整个Fontan术后随访期间,第二、第三和第四个十年的新发LC的年发病率分别为0.14%、0.43%和8.83%。LC患者的随访时间较长,AFP(甲胎蛋白)水平较高,肝纤维化指数值较高(P<0.01–0.0001)。此外,所有指标均可预测新发LC(P<0.01–0.0001)。LC治疗包括手术切除(n=3)、经动脉化学栓塞(n=3)、射频消融(n=2)和临终关怀(n=2)。在9.4个月的中位随访期间,有4例患者死亡。1年生存率为60%,无症状患者生存率更好(P <0.01)。
由此可见,在Fontan手术30年后,LC的发生率迅速增加,肝纤维化指标和AFP可作为新发LC的预测指标。应严格监控这些LC预测标记物,以尽早发现LC和改善患者预后。
原始出处:
Hideo Ohuchi.et al.Incidence, Predictors, and Mortality in Patients With Liver Cancer After Fontan Operation.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.120.016617
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#发病率#
74
#Fontan#
0
#AHA#
99
#预测指标#
71
#Fontan手术#
74
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
78
学习了
0