NEJM:利拉鲁肽可降低2型糖尿病患者心血管疾病发生率
2016-06-17 MedSci MedSci原创
研究人员通过进行研究后发现,利拉鲁肽可显著降低2型糖尿病患者心血管疾病的风险。该研究是第二项由FDA授权进行的关于糖尿病药物对糖尿病患者心血管安全性的相关研究,有助于医生更好地帮助糖尿病患者选择治疗药物。该研究由德克萨斯大学西南医学中心的Steven P Marso博士和同事共同开展,研究结果发表于NEJM。利拉鲁肽可降低机体糖化血红蛋白水平、体重并导致机体易出现低血糖,常见的不良反应有胃肠道反应
研究人员通过进行研究后发现,利拉鲁肽可显著降低2型糖尿病患者心血管疾病的风险。该研究是第二项由FDA授权进行的关于糖尿病药物对糖尿病患者心血管安全性的相关研究,有助于医生更好地帮助糖尿病患者选择治疗药物。该研究由德克萨斯大学西南医学中心的Steven P Marso博士和同事共同开展,研究结果发表于NEJM。
利拉鲁肽可降低机体糖化血红蛋白水平、体重并导致机体易出现低血糖,常见的不良反应有胃肠道反应和心率加快。虽然大多数研究人员将二甲双胍作为首选药物,但是这些研究结果也有助于研究人员开启里程碑式的研究,并致力于探究出可用于选择的二线药物。
谢菲尔德大学的Simon Heller博士指出,许多糖尿病患者死于低血糖,这应引起我们的重视,利拉鲁肽和empagliflozin都不会导致患者发生低血糖和其他不良反应。但是研究人员仍需进行更进一步的研究。
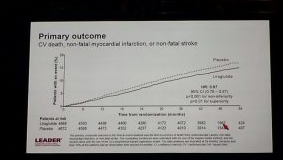
研究人员于2010年对9340名患2型糖尿病且具有心血管疾病高风险的民众进行了3.5-5年的随访研究,LEADER实验参与的2型糖尿病患者糖化血红蛋白水平高于7.0%,年龄均超过50岁且具有心血管疾病或肾功能不良,或年龄超过60岁且有患心血管疾病风险因素。受试者平均年龄为64岁,糖尿病史为13年,平均糖化血红蛋白水平为8.7%。研究人员将他们随机分为2组,实验组民众每天皮下注射利拉鲁肽1.8 mg(或可允许的最大剂量),对照组民众接受标准治疗。主要治疗目标是患者的糖化血红蛋白水平、血压、血脂调节和抗血小板治疗。研究人员关注的主要结果是民众出现主要不良心血管事件(MACE)的发生率,包括:心血管疾病死亡、非致死性心肌梗死(MI)或者非致命性卒中。
36个月的观察和治疗后,研究人员发现,实验组患者糖化血红蛋白水平下降了0.4%(P<0.001),体重也明显下降,平均减轻2.3kg(P<0.001)。实验组患者MACE发生率降低13%(发生率为608/4668),对照组为14.9%(发生率为694/4672,优势比P=0.01),实验组患者心血管疾病死亡率降低22%(4.7 vs 6.0%,P=0.007)。MI发生率也降低12%(6.0%vs6.8%,P=0.11),非致死性卒中发生率降低11%(3.4%vs3.8%,P=0.30),全因死亡率降低15%(8.2%vs9.6%,P =0.02),心衰住院率降低13%(4.7%vs5.3%,P=0.14)。研究人员认为这些数据十分有意义。从某一角度而言,利拉鲁肽可降低2型糖尿病患者心血管疾病的发生率。两组患者视网膜病变发生率无明显区别。
研究人员表示仍需进行更进一步的研究,以探究利拉鲁肽对2型糖尿病患者血流动力学变化的影响。
原始出处:
1.Miriam E Tucker. 'New Era' of Type 2 Diabetes Treatment as LEADER Unveiled? Medscape.2016 June 13.
2.Steven P. Marso,et al. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. NEJM.2016 June 13.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#发生率#
84
文章很好,非常有益
97
好文拜读了,认真学习了。
103
己拜读,受益匪浅
97
好文章,百姓也能从中学到好多医学知识
0
#2型糖尿病患者#
42
#糖尿病患者#
45
#血管疾病#
61