Hypertension:常用的量血压方法竟“不靠谱”!年纪越大越不准……
2020-03-14 王继光 马克洪峰 医学界心血管频道
众所周知,血压是众多心脑血管疾病的主要风险因素,上臂袖带法是临床和日常生活中我们最常使用的血压测量方法。
众所周知,血压是众多心脑血管疾病的主要风险因素,上臂袖带法是临床和日常生活中我们最常使用的血压测量方法。
而近期,《高血压(Hypertension)》上发表了一项国际有创血压合作研究给出了不同的看法,中国高血压联盟主席、上海交通大学医学院附属瑞金医院的王继光教授是研究作者之一。
这项研究发现,在老年人中,上臂袖带血压值并不能够准确反映真实动脉系统血压,而且随着年纪增长,准确率也在逐渐下降。

文章标题:《年龄因素对上臂袖带血压测量的影响》
研究究竟是怎么说的,一起来看看吧。
年龄越大,
上臂袖带血压值越不准!
这一研究纳入了1674位受试者,平均年龄为64岁,32%为女性,所有受试者均接受了冠脉造影,使用有创动脉导管测量动脉血压(全部受试者测量主动脉血压,部分加测肱动脉血压),并同步采集上臂袖带血压测量数据,研究中共用到了22种不同的上臂袖带血压检测仪器,包括19种示波血压计、1种自动听诊血压计和2种水银血压计。
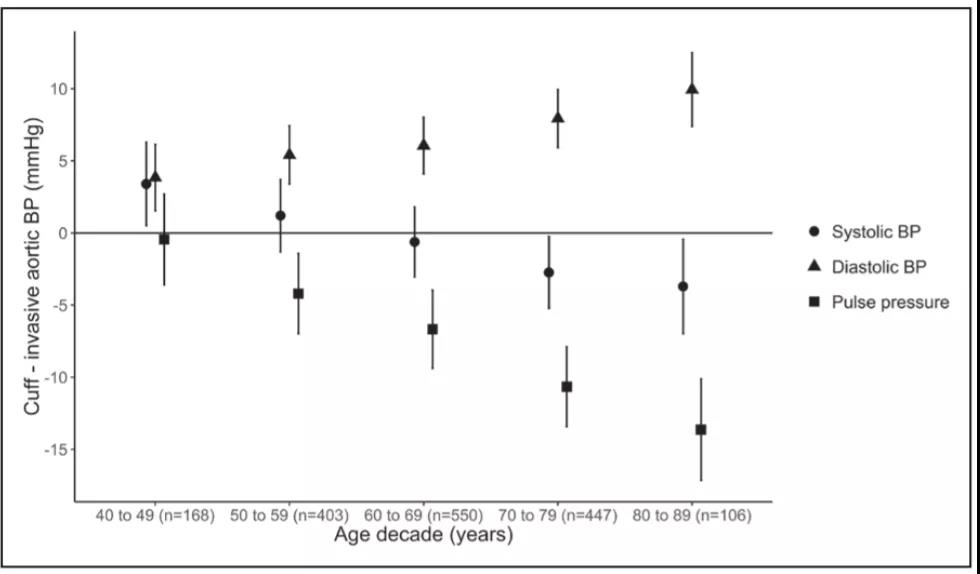
图1:不同年龄段人群中上臂袖带血压与主动脉实际血压之间的差值
图中的圆点为收缩压、三角形为舒张压、正方形为脉压差。点值距基线越远意味被错误估计的程度越大。
从图1中可以看到,在50岁及以上的受试者中,随着年龄增长,上臂袖带法测量的收缩压数值逐渐低于实际主动脉收缩压(P<0.0001 ),年龄越大,这种趋势越明显。
相反,通过上臂袖带检测的舒张压,则高于主动脉实际舒张压(P<0.0001 ),且随着年龄增长,高出的幅度越来越大。
要知道,与周围动脉血压,如肱动脉血压相比,主动脉血压能更好反映人体主要脏器的血流灌注情况,是评估心血管事件更为有效的指标。因此,随着年龄增长,通过上臂袖带检测获得的脉压差(收缩压和舒张压之差),逐渐低于主动脉实际脉压差(P<0.0001 )。
即使在校正了年龄、平均动脉压、心率、体重指数(BMI)等因素后,上臂袖带血压测量值与主动脉实际血压之间的差异仍然是有意义的(P<0.0001 ),而有创测量方式保证了动脉血压的真实准确性。因此,研究者将有创主动脉血压作为参考标准,在年龄分层下,将受试者上臂袖带血压与其进行比较。
研究者将520名受试者的上臂袖带血压值和有创肱动脉血压进行了比较,结果提示,老年人的袖带血压同样不能准确反映肱动脉真实血压值,年龄越大,二者差异越明显。
研究者还发现处于不同血压范围的受试者,其上臂袖带血压与主动脉实际血压之间的差异与全体差异趋势一致。
那么,年龄因素影响袖带血压测量的原因是什么呢?研究者对年龄影响上臂袖带测量法估计真实血压情况的可能原因做了简单讨论,比如心率、血管顺应性等因素,但并无定论,也强调这并不是本项研究的目的。
上臂袖带血压不准,
有何后果?
我们都知道,正确测量血压在恰当评估和控制心血管病风险时至关重要。如果该项研究结果在人群中得到进一步确证,那对于老年人来说,最直接的影响,是可能会导致与血压相关的各种实际风险被错误估计,影响临床诊断、干预措施的实施及疗效评估等。
另一方面,在目前世界最重要的几项血压相关流行病学研究中,是通过上臂袖带法采集血压值的,而根据有创血压合作研究的结论,这些研究中对血压关联强度的评估会受到影响,增加了临床诊断和血压控制目标的不确定性。
再者,这也会影响新型血压测量设备的验证方案制定。
怎么办?
有了铺路者,后面人的路会好走
无法否认,几十年来,上臂袖带血压测量在成年人的心血管疾病风险评估中起到了重要作用,但通过该方法获得的血压值对整个动脉系统而言毕竟是粗略的,不够精确的。有创血压合作研究的新发现,使人们更深入地理解血压随年龄变化的趋势,为后续相关研究及新型血压测量仪器的研发提供了依据。
相信在科技快速发展的当代,血压测量方法会得到不断的改良创新,期待出现既如袖带测量法般简便易行,又能够有效排除年龄等混杂因素影响,更准确地反映真实血压数值的测压“神器”,以改善心血管病的预防和治疗。
至此,笔者想说的是,动脉血压数值金标准是通过动脉导管的放置来获得的,这是一项有创性的操作,需要专业有经验的医生进行,且对设备环境有特殊要求。
在更好的血压测量仪器或方法推出之前,上臂袖带法测量血压仍是目前最易实施操作、快速、经济的测血压方法,其在普查、病情初判、患者自我管理等方面的地位无法取代。
所以,各位老年高血压患者,请继续规范使用袖带测压计规律监测您的血压,毕竟目前情况下,有创测量主动脉血压,不是你想测,想测就能测!
专家简介
 王继光 教授
王继光 教授
王继光,医学博士,上海交通大学医学院心血管内科学博士生导师,上海交通大学公共卫生学院博士生导师。上海市高血压研究所所长,上海交通大学医学院附属瑞金医院高血压科主任、瑞金北院高血压科主任。主要从事高血压诊治与研究工作。亚太高血压学会(APSH)主席,The HOPE Asia Network副主席,中国高血压联盟(CHL)主席,中国医师协会高血压专业委员会副主任委员。国际高血压学会前执委,亚洲动脉学会(POA)前主席。Hypertension杂志副主编,Hypertension Research杂志副主编。《中华心血管病杂志》副总编,《中华高血压杂志》副主编。截至2019年11月19日,全文发表英文论著或综述424篇,中文论著与综述161篇。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







_1583674014000.jpeg)








#量血压#
69
#TENS#
67
#PE#
80
学习了
124
#靠谱#
126
#Hypertension#
83