Circulation:电解剖电位图在心肌内膜活检中的诊断价值
2020-10-03 星云 MedSci原创
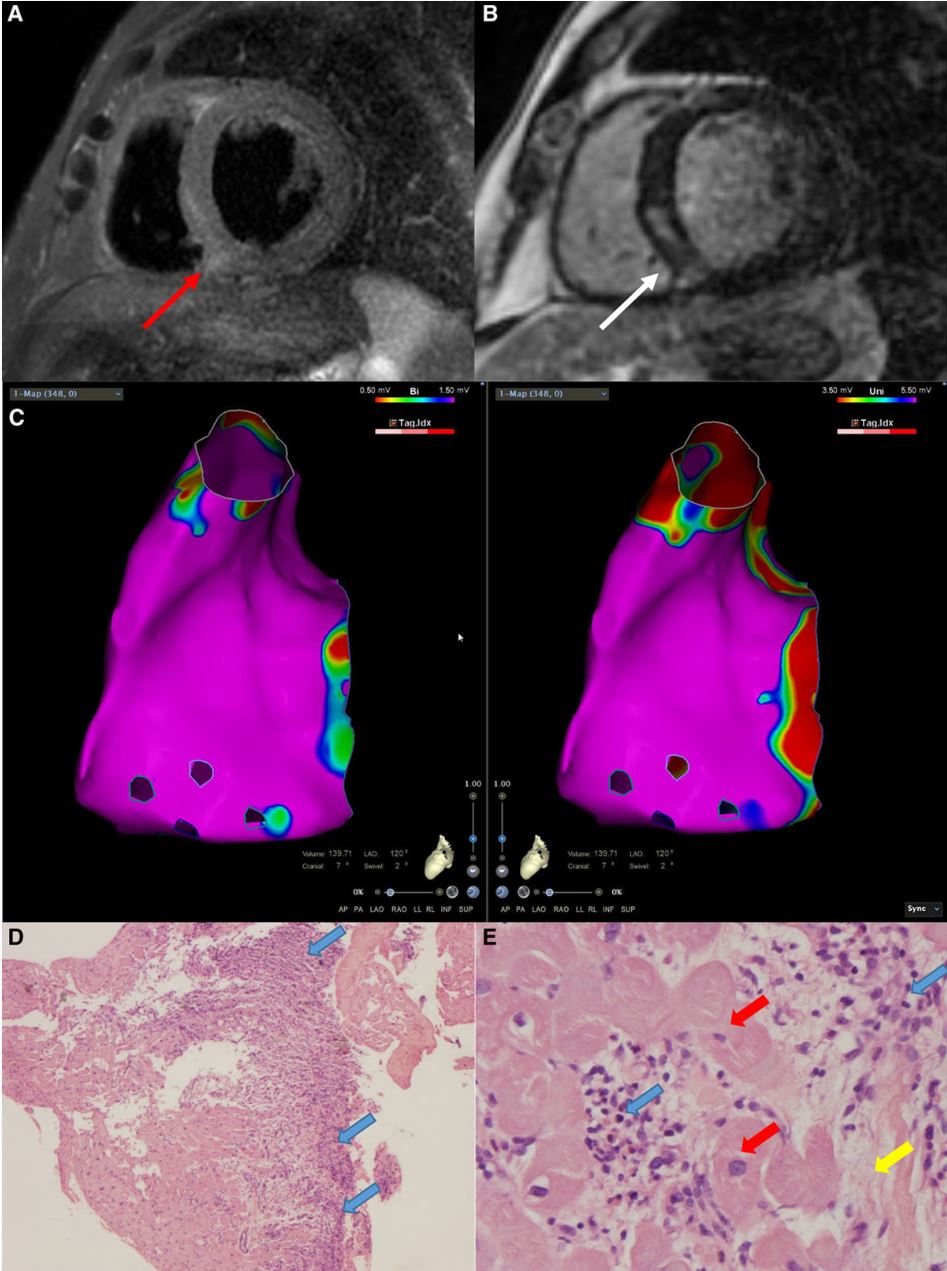
电解剖电位图(EVM)是一种很有前途的心肌内膜活检(EMBs)方法。然而,目前很少有数据支持其可行性和安全性。本研究报告了接受EVM引导的EMBs的最大患者队列,以显示其诊断效果,并将其与心脏磁共振(
该队列共纳入了162位患者(2010年-2019年)。在EVM和CMR确认的病理区域进行EMB。根据EMB结果评估CMR和EVM在鉴别心肌病变部位的敏感性和特异性。
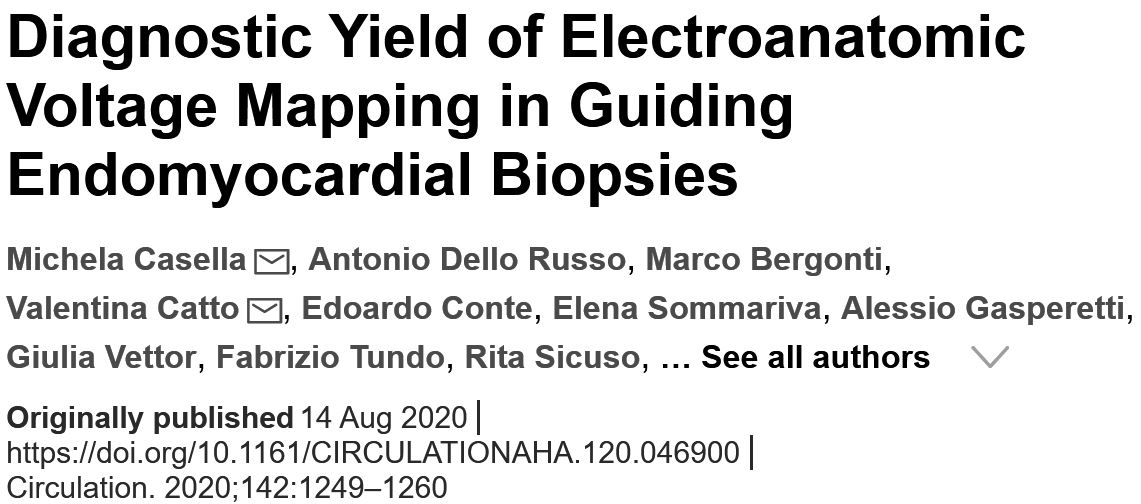
ARVC合并心肌炎一例
术前CMR显示有70%的患者有晚期钆增强,而EVM提示有61%的患者存在低压区。右心室(73%)、左心室(19%)或双侧心室(8%)取样。EVM被证明与CMR具有相似的敏感性(74% vs 77%),特异性分别为70%和47%。
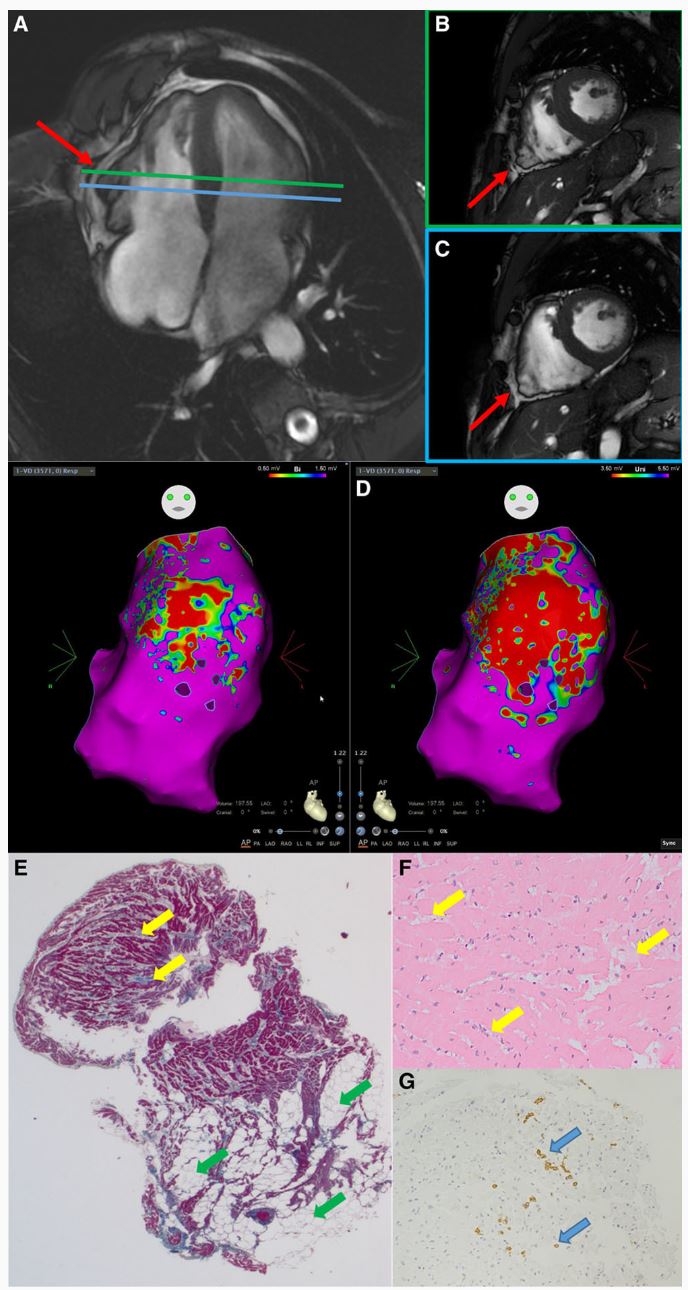
嗜酸性心肌炎一例
在12例经EMB证实的心肌病患者中,EVM发现了CMR评估中未发现的病理区域。EVM和CMR合用的灵敏度高达95%。EMB分析使39%的患者明确诊断,与疑诊区分开来。并发症发生率低,大多与血管通路有关,无患者需要紧急处理。
综上,鉴于EVM对心肌病变区域的敏感性和特异性,它被证明是一种很有前途的靶向EMB工具。EVM具有与CMR相似的精确度。EVM联合CMR对EMB的阳性预测值高达89%。
原始出处:
Michela Casella, et al. Diagnostic Yield of Electroanatomic Voltage Mapping in Guiding Endomyocardial Biopsies. Circulation. 2020;142:1249–1260
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#诊断价值#
93
#内膜#
63
马住
133
#活检#
61
棒
123
#心血管#又是新的研究方向
174