Ann Hematol:19 种药物疗法对特发性血小板减少性紫癜患者的疗效比较
2022-02-16 MedSci原创 MedSci原创
安慰剂、口服免疫抑制剂和地塞米松加奥司他韦的效果不如其他测试的 ITP 疗法。开始治疗 ITP 时,艾曲波帕加利妥昔单抗可能是最佳选择。
 免疫性血小板减少症(ITP)是临床上最常见的出血性疾病,重症患者死亡率高,长期生存质量差。其治疗方案多样,但关于如何选择合适的治疗方法目前尚存在争议。有一项荟萃分析研究系统回顾了 2015 年 1 月 1 日-2021 年 4 月 20 日期间的 19 项随机对照试验(包括 2615 名参与者),目的是提供一个临床有用的总结,用于指导治疗决策。
免疫性血小板减少症(ITP)是临床上最常见的出血性疾病,重症患者死亡率高,长期生存质量差。其治疗方案多样,但关于如何选择合适的治疗方法目前尚存在争议。有一项荟萃分析研究系统回顾了 2015 年 1 月 1 日-2021 年 4 月 20 日期间的 19 项随机对照试验(包括 2615 名参与者),目的是提供一个临床有用的总结,用于指导治疗决策。
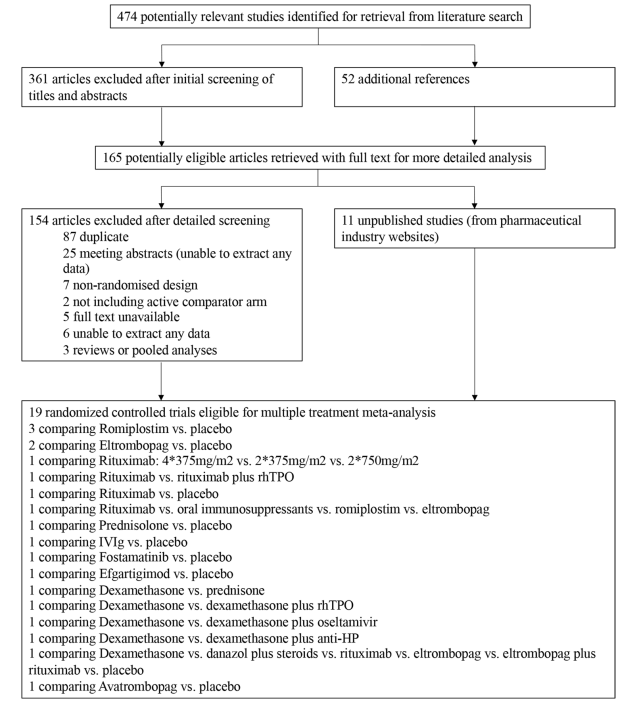
图1:研究选择过程:45组对应的19项随机对照试验纳入本多治疗荟萃分析
这些研究比较了治疗剂量范围内的多种药物或其组合治疗 ITP。主要终点是基于对这些疗法有反应的患者比例。
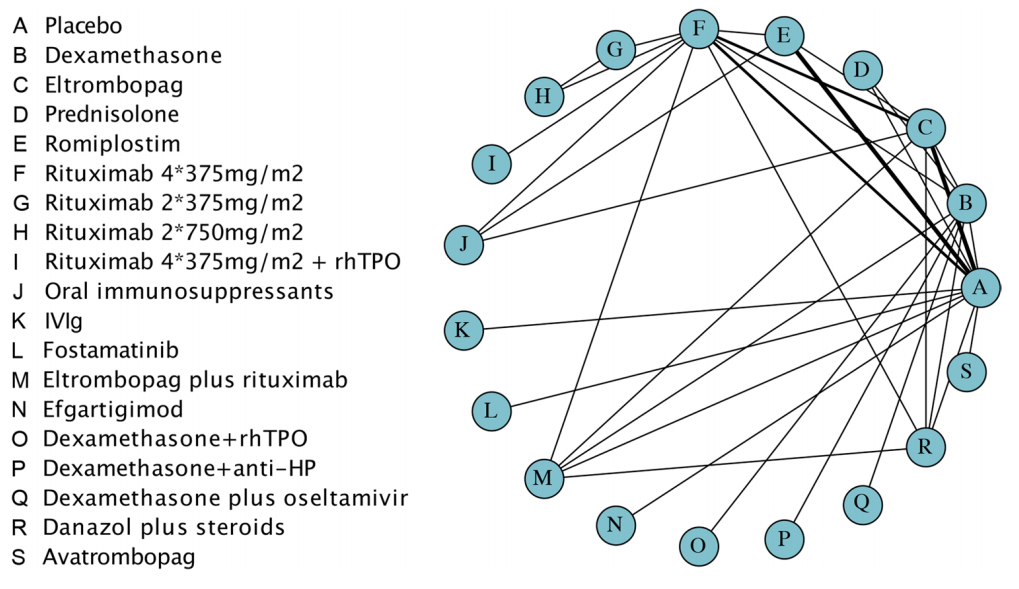
图2:多治疗治疗(应答率)荟萃分析比较网络。该线的宽度与比较每个治疗对的试验次数成正比
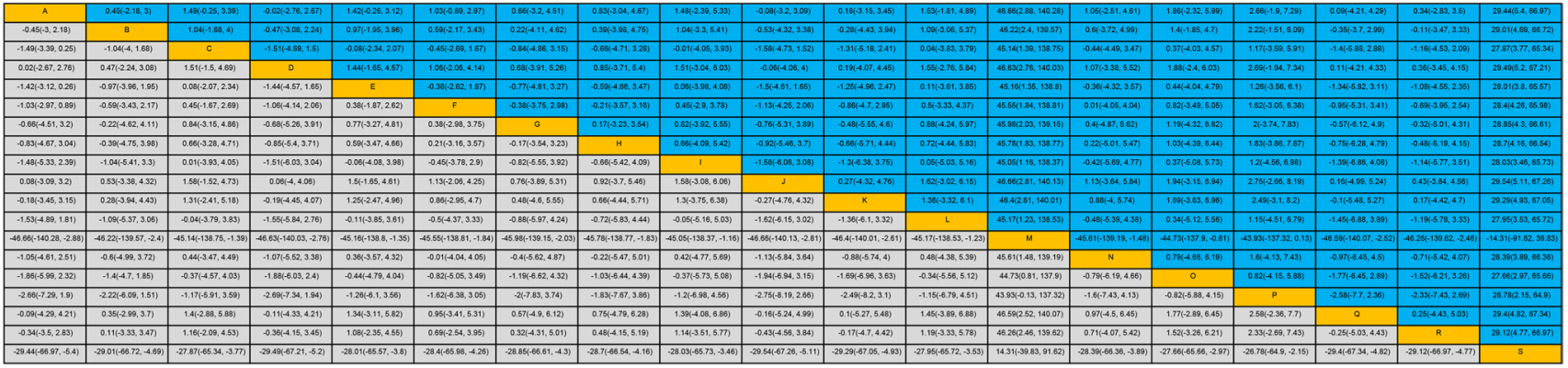
图3:19种ITP治疗方法的疗效按字母顺序排列。A=安慰剂。B=地塞米松。C=艾曲波帕。D=泼尼松龙。E=罗米倍体。F=利妥昔单抗 4*375 mg/m2 .G=利妥昔单抗 2*375 mg/m2 .H=利妥昔单抗 2*750 mg/ m2 .I=利妥昔单抗4*375mg/m2+rhTPO。J=口服免疫抑制剂。K=IVIg。L=福坦替尼.M=艾曲波帕加利妥昔单抗。N=efgrigimod。O=地塞米松加rhTPO。P=地塞米松加抗hp。Q=地塞米松加奥司他韦。R=达那唑加类固醇。S=阿瓦托巴格。
艾曲波帕加利妥昔单抗、阿瓦曲波帕、地塞米松加抗HP、地塞米松加rhTPO的疗效显着高于安慰剂(OR46.66、29.44、2.66、1.86) 或单独使用地塞米松 (OR46.22, 29.01, 2.22, 1.40)。
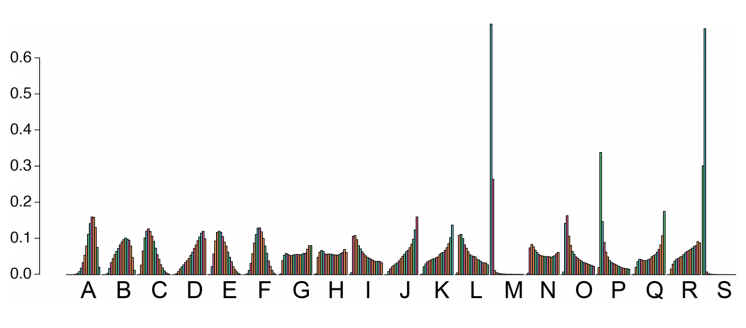
图4:Efcacy排名。该排名表明了19种ITP治疗方案中的每一种都将是最好到最坏的方案的可能性。例如,方案M:艾曲波帕加利妥昔单抗,它有超过90%的可能性排在第一,所以这个方案大概是19种方案中最有效的
各研究之间使用的推断终点不一定相同,这是该荟萃分析中异质性的主要来源。同时,由于荟萃分析中包含的文章来自于所纳入人群的不完全一致性,这可能会产生一定数量的异质性。未来的面对面的临床试验仍然需要获得更好的验证。
总的来说,安慰剂、口服免疫抑制剂和地塞米松加奥司他韦的效果不如其他测试的 ITP 疗法。开始治疗 ITP 时,艾曲波帕加利妥昔单抗可能是最佳选择。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#特发性血小板减少性紫癜#
80
#特发性#
76
#血小板减少性紫癜#
74
#药物疗法#
89
赞
87
感谢分享
93
#血小板减少#
119
#EMA#
67
#紫癜#
80
赞
80