Int J Cardiol:术前全身CT扫描与微创二尖瓣手术中卒中风险降低相关
2018-12-13 xing.T MedSci原创
由此可见,术前全身CT筛查与较低的术后卒中风险和透析需求以及MIMVS后手术死亡率降低的趋势相关。
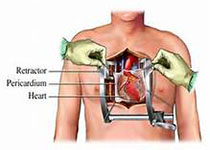
微创二尖瓣手术(MIMVS)在临床进行的频率越来越高。然而,接受MIMVS治疗的患者围手术期卒中的风险可能增加,这主要是由于股动脉-心肺转流术中逆行主动脉栓塞所致。术前计算机断层扫描(CT)筛查可做到主动脉和股髂血管的可视化和手术方法的个性化。近日,心血管领域权威杂志International Journal of Cardiology上发表了一篇研究文章,在这项荟萃分析中,研究人员的目标是确定全身性术前CT筛查是否与MIMVS术后卒中和其他并发症发生率降低有关。
研究人员对PubMed(从成立至2018年5月)进行了全面的审查。符合条件的研究包括报告MIMVS和逆行动脉灌注的研究。研究分为两个亚组:全身术前CT筛查(CT组)和无CT筛查(非CT)。研究人员评估了手术死亡、术后卒中、围手术期心肌梗死(MI)和需要透析的新发肾衰竭汇总事件发生率(PER),并进行组间比较。
研究人员分析了来自57项研究(13731名患者)的数据(19个CT组,38个非CT组)。术后卒中的PER为2.0%,两组间差异具有统计学意义(CT组:1.5% vs. 非CT组:2.2%,P=0.03)。新透析的PER为1.9%,在CT组显著降低(0.8% vs. 非CT组为2.3%,P=0.02)。手术死亡率的PER为1.4%,CT组的结局趋势更好(非CT组为0.8% vs. 1.6%,P=0.05)。
由此可见,术前全身CT筛查与较低的术后卒中风险和透析需求以及MIMVS后手术死亡率降低的趋势相关。
原始出处:
Jeremy R.Leonard,et al.Systematic preoperative CT scan is associated with reduced risk of stroke in minimally invasive mitral valve surgery: A meta-analysis.International Journal of Cardiology.2018.https://doi.org/10.1016/j.ijcard.2018.12.025
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#风险降低#
61
#Cardiol#
69
#二尖瓣手术#
83
#卒中风险#
69
#微创#
65
#二尖瓣#
56
#CT扫描#
89
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
94
中风是俗称,应该称为缺血性卒中吧
114