Front Med:亚洲人急性肺栓塞后慢性血栓栓塞性肺动脉高压的发生率高于欧洲人
2021-11-14 刘少飞 MedSci原创
急性肺栓塞后慢性血栓栓塞性肺动脉高压(CTEPH)的发生率为3%,亚洲人的发病率高于欧洲人。应努力早期诊断和治疗 PE 患者,尤其是高危人群的 CTEPH。

慢性血栓栓塞性肺动脉高压 (CTEPH) 是一种独特的肺动脉高压 (PH),其特征在于肺动脉血栓的纤维化转化、肺动脉的固定阻塞和高肺血管阻力。在临床上,晚期患者经常CTEPH有权心脏衰竭的症状严重,如果不治疗(这些病人的临床结果都很差)。目前对 CTEPH 患者的治愈性治疗主要是肺动脉内膜切除术 (PEA),这与提高这些患者的生存率有关。然而,CTEPH 患者的临床表现大多是非特异性的,难以与肺栓塞 (PE) 的症状相鉴别。因此,CTEPH 的早期诊断仍然是当前临床实践中的一个挑战。因此,对于PE患者进行 CTEPH 常规筛查是否具有合理性仍然不确定,并且根据之前的研究,急性PE后患者的 CTEPH 发生率仍然存在差异。虽然之前发表的两项荟萃分析总结了急性 PE 患者 CTEPH 的发生率,但仅纳入了 2018 年之前发表的研究。一些最近发表的临床试验不包括。此外,尚不清楚患者和研究特征(例如患者种族、研究设计或样本量)是否会显着影响 CTEPH 的发生率。此外,虽然之前有静脉血栓栓塞事件 (VTE) 或无端 PE 的患者被认为是 CTEPH 的高危患者,之前的荟萃分析中尚未对这些风险因素的几率进行定量分析。因此,在本研究中,我们旨在总结急性 PE 后右心导管诊断为 CTEPH 的发生率,并在更新的荟萃分析中探讨其影响因素,并探讨患者和研究特征对结果的潜在影响。
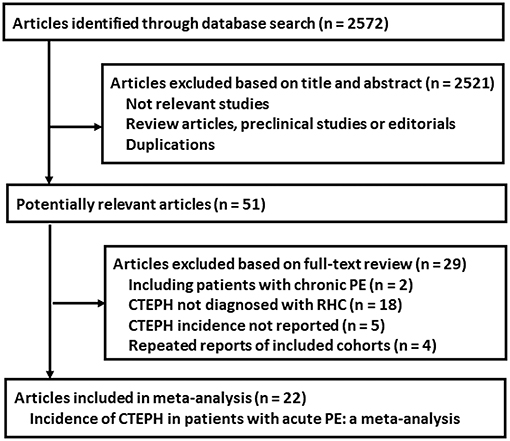
文献检索和研究鉴定的过程
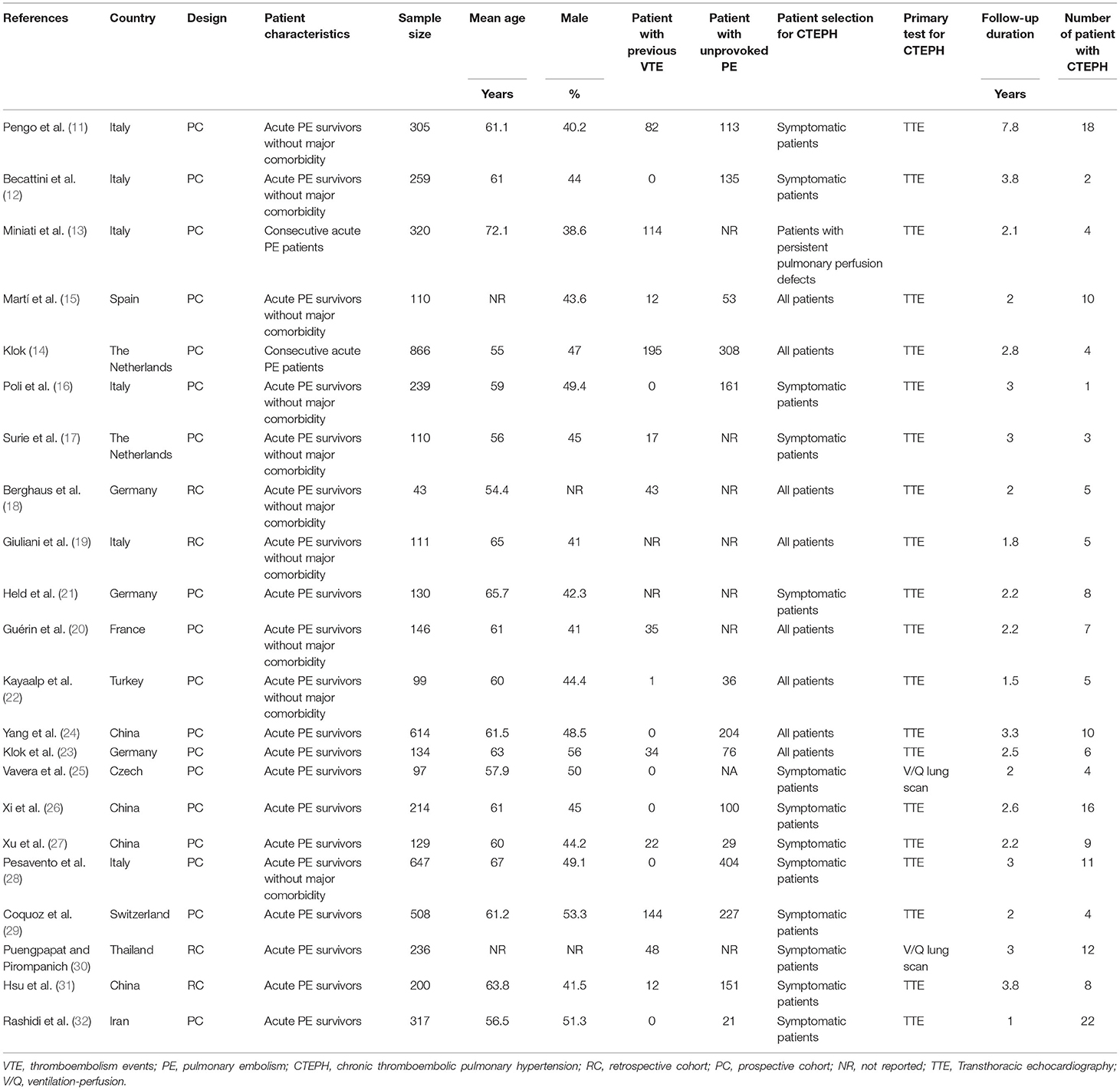
研究特点和质量评价
共纳入22 项队列研究,涉及 5,834 名急性 PE 患者。纳入队列的基线特征见表1。这些研究是2004年至2020年间出版,并在意大利,西班牙,荷兰,德国,法国、土耳其、捷克、瑞士、中国,泰国,和伊朗。纳入的研究中有 18 项为前瞻性队列研究,而其他 4 项为回顾性研究。每项研究纳入的急性PE患者人数从43到866不等。患者的平均年龄从54到72岁不等,男性患者的比例从38%到56%不等。平均随访 2.9 年,174 名患者被诊断为 CTEPH。所有纳入的患者在 8 项研究的随访期间均接受了 CTEPH 筛查,而其他 14 名一般选择有症状的患者进行 CTEPH 筛查。大多数纳入的研究使用经胸超声心动图 (TTE) 作为 CTEPH 筛查的主要测试,除了两项应用 V/Q 肺扫描的研究。
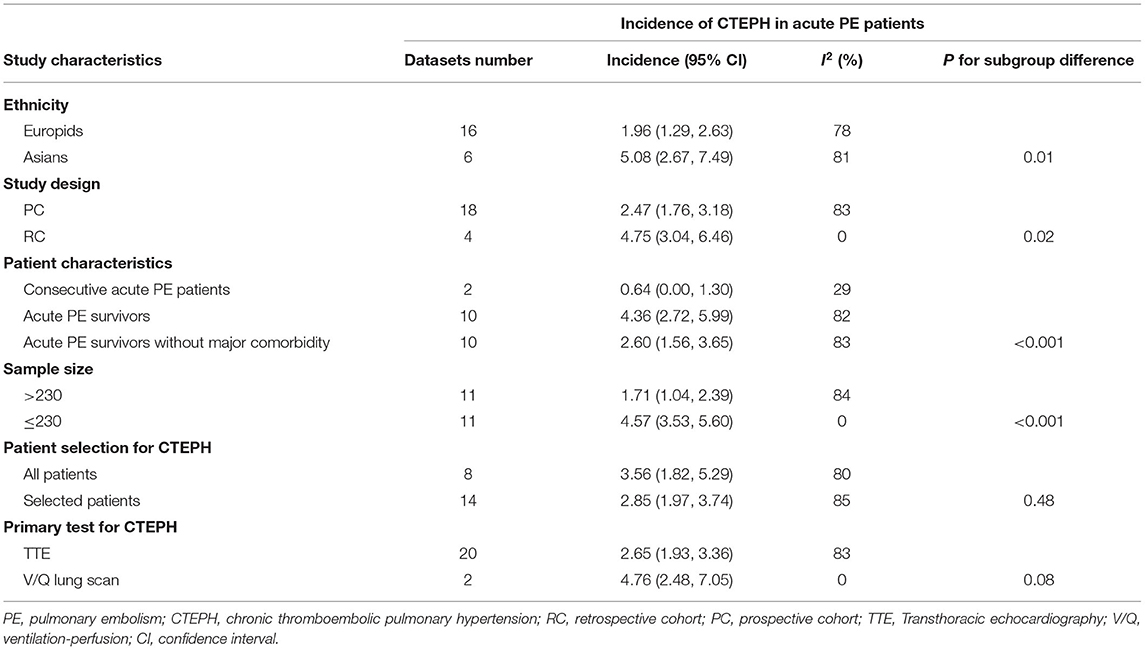
急性 PE 患者 CTEPH 的发生率
荟萃分析中包括的各个队列中报告的急性 PE 患者 CTEPH 的发生率在 0.42% 和 11.63% 之间变化。注意到显着的异质性(Cochrane 的Q检验的p < 0.001,I 2 = 82.8%)。将 22 个队列的结果汇总显示,CTEPH 的总体发生率为 2.82%(95% 置信区间:2.11-3.53%;图 2)。亚组分析显示亚洲人 CTEPH 的发生率高于欧洲人(5.08 对 1.96%,p = 0.01),在回顾性队列中高于前瞻性队列(4.75 对 2.47%,p = 0.02),并且在样本量小于那些的研究中样本量更大(4.57 vs. 1.71%,p< 0.001; 表 3 )。亚组分析还显示,连续急性 PE 患者的 CTEPH 发生率为 0.64%(95% CI:0.00-1.30%),急性 PE 幸存者为 4.36%(95% CI:2.72-5.99%),2.60%(95在没有严重合并症的急性 PE 幸存者中,% CI:1.56–3.65%(表下)。在所有 PE 患者或选定的 PE 患者中筛查 CTEPH,或使用 TTE 或 V/Q 肺扫描作为一线检测似乎并未显着影响报告的急性 PE 后 CTEPH 的发生率(p > 0.05)。
研究总结:
在这项队列研究的荟萃分析中,通过汇总更新的队列研究结果,我们发现急性 PE 后患者 CTEPH 的总体发生率为 2.82%。按患者特征进行的亚组分析显示,在对连续急性 PE 患者的研究中,CTEPH 的发生率为 0.64%,在急性 PE 幸存者中为 4.36%,在没有主要合并症的急性 PE 幸存者中为 2.60%。亚组分析还显示,亚洲人 CTEPH 的发生率高于欧洲人(5.08% 对 1.96%),在回顾性队列中高于前瞻性队列(4.75% 对 2.47%),在样本量较小的研究中比样本量较大的研究(4.57 对 2.47%) . 1.71%),而在所有 PE 患者或选定的 PE 患者中筛查 CTEPH,或使用 TTE 或 V/Q 肺扫描作为一线测试似乎没有显着影响报告的发生率。此外,分层分析表明,既往静脉血栓栓塞事件和无端 PE 均与 CTEPH 风险增加显着相关。综上所述,这项更新的荟萃分析的结果表明,急性 PE 后 CTEPH 的发生率约为 3%,亚洲人的发生率可能高于欧洲人,尽管这可能受患者特征和研究设计因素的影响。应努力早期诊断和治疗 PE 患者,尤其是高危人群的 CTEPH。尽管它可能会受到患者特征和研究设计因素的影响。应努力早期诊断和治疗 PE 患者,尤其是高危人群的 CTEPH。尽管它可能受患者特征和研究设计因素的影响。应努力早期诊断和治疗 PE 患者,尤其是高危人群的 CTEPH。
文献出处:
Pang W, Zhang Z, Wang Z, Zhen K, Zhang M, Zhang Y, Gao Q, Zhang S, Tao X, Wan J, Xie W, Zhai Z. Higher Incidence of Chronic Thromboembolic Pulmonary Hypertension After Acute Pulmonary Embolism in Asians Than in Europeans: A Meta-Analysis. Front Med (Lausanne). 2021 Oct 26;8:721294. doi: 10.3389/fmed.2021.721294. PMID: 34765615; PMCID: PMC8575791.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#发生率#
71
#动脉高压#
54
#急性肺栓塞#
62
#欧洲#
69
#Med#
107