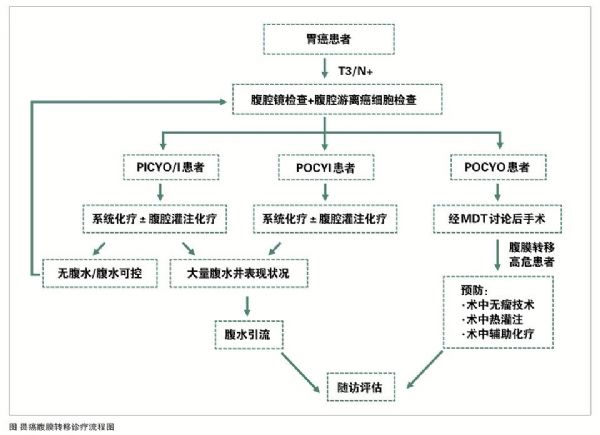
《胃癌腹膜转移防治中国专家共识》颁布——推动胃癌腹膜转移的规范化诊断与治疗
2017-07-20 CMT 中国医学论坛报
本次共识基于既往循证医学研究和临床实践,综合我国胃癌领域百余位专家的科研及临床经验进行撰写,具有简单实用、科学严谨和普适性等特点,从腹膜转移的诊断与分期、预防的主要手段及发生腹膜转移后的治疗等方面进行诠释,以期让广大临床医师更好地理解并加以运用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#胃癌腹膜转移#
84
#诊断与治疗#
58
#规范化#
59
#中国专家共识#
71
#专家共识#
67
学习了,谢谢
107
#腹膜转移#
92
#腹膜#
71
学习了谢谢分享
114