NEJM:血栓切除术,做还是不做?( TOTAL试验)
2015-03-20 MedSci MedSci原创
背景:在主要经皮冠状动脉脉介入治疗即PCI治疗中,手动血栓切除术可以减少远端血栓的存在从而改善微循环灌注,小规模试验表明血栓切除术可以改善替代治疗和临床效果,但是稍复杂的试验则会出现有争议的临床结果。研究方式:我们随机分配10732位ST段抬高型心肌梗死即STEMI的患者接受两种治疗:常规PCI治疗(对照组)和进行手动血栓切除术后进行PCI术(即实验组)。我们关注的主要指标是:心血管疾病原因导致的
背景:

研究方式:
我们随机分配10732位ST段抬高型心肌梗死即STEMI的患者接受两种治疗:常规PCI治疗(对照组)和进行手动血栓切除术后进行PCI术(即实验组)。我们关注的主要指标是:心血管疾病原因导致的死亡患者人数、复发性心肌梗塞和心源性休克的人数、180天内根据纽约心功能分级4级心脏衰竭的患者人数、30天内发生中风的患者人数。
结果:
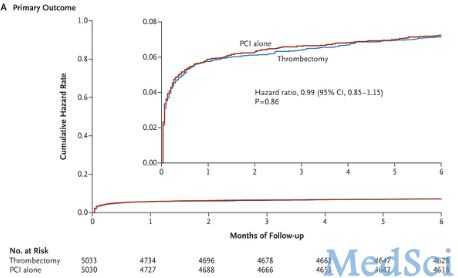
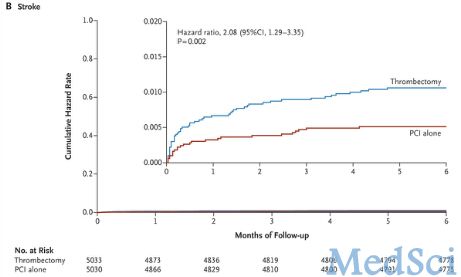
主要结果体现在实验组5033例患者中的347例和对照组的5030例患者中的351例(血栓切除术的危险比为0.99,95%的可信区间为0.85到1.15,P=0.86)。实验组由于心血管疾病导致的死亡患者占3.1%,对照组所占比例为3.5%,危险比为0.90,95%的可信区间为0.73到1.12,P=0.34。支架内血栓形成或靶血管血运重建的比例在实验组和对照组分别为9.9%和9.8%,危险比为1.00,95%可信区间为0.89到1.14,P=0.95,结果相差不大。30天内实验组发生中风的患者有33位,占0.7%,对照组有16位患者,占0.3%,危险比为2.06,95%可信区间为1.13到3.75,P=0.02.
结论:
发生STEMI并接受血栓切除术后接受常规PCI治疗的患者相比进行常规PCI治疗的患者而言,并不能降低心血管疾病导致患者死亡、复发性心肌梗塞和心源性休克的风险,也不能减少180天内根据纽约心功能分级4级心脏衰竭的患者人数,但是却可以增加30天内发生中风的患者人数。由此看来,手动血栓切除术还是不做较为安全。
Jolly SS1, Cairns JA, Yusuf S, Meeks B, Pogue J, Rokoss MJ, Kedev S, Thabane L, Stankovic G, Moreno R, Gershlick A, Chowdhary S, Lavi S, Niemelä K, Steg PG, Bernat I, Xu Y, Cantor WJ, Overgaard CB, Naber CK, Cheema AN, Welsh RC, Bertrand OF, Avezum A, Bhindi R, Pancholy S, Rao SV, Natarajan MK, Ten Berg JM, Shestakovska O, Gao P, Widimsky P, Džavík V; TOTAL Investigators.Randomized Trial of Primary PCI with or without Routine Manual Thrombectomy.N Engl J Med. 2015 Mar 16. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Total#
117
#切除术#
77
#血栓切除#
97
#血栓切除术#
145
这个研究值得学习
160