Dent Mater:抗菌药打得赢氧化锆表面生物膜么?
2017-04-06 MedSci MedSci原创
二氧化锆在美学上具有明显的优势,近年来在临床中上的使用越来越广泛,但其生物性能,尤其是否会引起种植体周围相关炎症、或者在种植体周围相关炎症发生后抗菌药物是否有效,这些问题仍需探究。为此,Sánchez MC等学者对纯钛和氧化锆表面生物膜对抗菌药的反应进行了研究。
二氧化锆在美学上具有明显的优势,近年来在临床中上的使用越来越广泛,但其生物性能,尤其是否会引起种植体周围相关炎症、或者在种植体周围相关炎症发生后抗菌药物是否有效,这些问题仍需探究。为此,Sánchez MC等学者对纯钛和氧化锆表面生物膜对抗菌药的反应进行了研究。
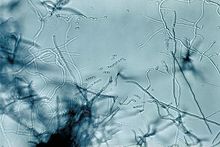
他们在喷砂酸蚀纯钛表面和二氧化硅表面形成体外生物膜,通过牙周致病菌数量的改变来评估抗菌药的效能。将两种表面的样本消毒并在其表面培养生物膜,模拟体内口腔环境。将培养72小时的生物膜浸入三种抗菌药:洗必泰/氯化十六烷基氨基吡啶(CHX/CPC)、香精油(EEOOs)和氯化十六烷基氨基吡啶(CPC),浸泡1分钟,并伴或不伴有机械清除作用。在叠氮碘化丙锭附着作用下通过qPCR检测活菌菌量。分别对伴放线放线菌、牙龈卟啉单胞菌和具核梭杆菌在每种表面上经不同药物处理后的活菌菌量变化建立广义线性模型,确定抗菌药在不同表面对不同牙周致病菌的抗菌效能。
结果发现:无论是喷砂酸蚀纯钛表面,还是二氧化锆表面,通过三种抗菌药作用,活菌菌量均有显着的下降。其中,对于伴放线放线菌,两种表面菌量上均降低2个数量级;对于牙龈卟啉单胞菌,喷砂酸蚀纯钛表面降低2个数量级,二氧化锆表面为3个数量级;对于具核梭杆菌,两种表面菌量减少值达到4个数量值。但暴露在单纯化学抗菌药或联合机械清除前后,喷砂纯钛表面和二氧化硅表面两种表面之间的菌量无统计学差异。
由此说明:尽管两种表面材料、结构不同,两种表面上所形成的混合菌菌落结构也存在差异,但伴放线放线菌、牙龈卟啉单胞菌和具核梭杆菌在两种表面上形成的混合菌生物膜对于抗菌药的反应都相似。
推想,在形成菌斑生物膜和抗菌药作用效能方面,二氧化锆和喷砂酸蚀表面可能无差异。
原始出处:
Sánchez MC, et al. Response to antiseptic agents of periodontal pathogens in in vitro biofilms on titanium and zirconium surfaces. Dent Mater.2017 33(4):446-453. doi: 10.1016/j.dental.2017.01.013.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#抗菌#
49
#抗菌药#
60
#氧化锆#
88
感谢分享一下!
90