Lancet:上海六院证实动态增强MRI能预测非小细胞肺癌骨转移患者的预后
2016-12-17 MedSci MedSci原创
骨转移是晚期非小细胞肺癌的一种常见并发症,骨转移引起的骨骼相关事件也导致了预后不良。而评估骨转移的治疗反应的标准方法目前尚不存在。近期,一篇发表在Lancet杂志上的研究应用了动态增强MRI获得定量指标来评估这项技术在使用长春瑞滨-顺铂联合重组人血管内皮抑素治疗以前未经治疗的非小细胞肺癌患者骨转移的治疗反应。研究者们在上海市第六人民医院做了4期、随机、前瞻性、双盲、安慰剂对照的临床试验。入选标准为
骨转移是晚期非小细胞肺癌的一种常见并发症,骨转移引起的骨骼相关事件也导致了预后不良。而评估骨转移的治疗反应的标准方法目前尚不存在。
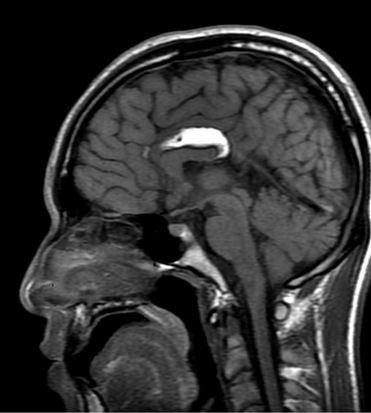
近期,一篇发表在Lancet杂志上的研究应用了动态增强MRI获得定量指标来评估这项技术在使用长春瑞滨-顺铂联合重组人血管内皮抑素治疗以前未经治疗的非小细胞肺癌患者骨转移的治疗反应。
研究者们在上海市第六人民医院做了4期、随机、前瞻性、双盲、安慰剂对照的临床试验。
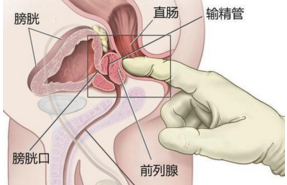
入选标准为经病理学或细胞学证实的非小细胞肺癌骨转移患者;影像资料表明有盆腔转移;年龄为18岁至75岁;预期存活时间至少3个月;未接受紫杉烷类、贝伐单抗、沙利度胺、重组人血管内皮抑素或双膦酸盐治疗;3个月内未接受放疗;常规血液检查结果正常;肝、肾功能及心电图正常;无心血管疾病、自身免疫性疾病、血管炎、严重感染、糖尿病等伴随疾病;并签署知情同意书。
排除标准为:在化疗期间接受粒细胞集落刺激因子或粒细胞巨噬细胞集落刺激因子;不能耐受不良反应;对造影剂过敏。
患者被随机分为治疗组和对照组。受试者接受长春瑞滨-顺铂联合重组人血管内皮抑制素或长春瑞滨-顺铂联合安慰剂治疗。长春瑞滨(25mg/m2)联合顺铂(75mg/m2)在第1天经静脉内给药(21天为一个周期)。患者在第1-14天接受重组人血管内皮抑制素(7.5mg/m2)或安慰剂治疗。
主要终点为客观缓解率(完全缓解+部分缓解)/总人数×100)以及疾病控制率(完全缓解+部分缓解+病情稳定)/总人数×100)。
动态增强MRI在治疗前和治疗后2个周期后评价测量值(Ktrans、Kep、Ve)。治疗前后测定骨代谢指标、肿瘤标志物及肿瘤血管生长相关因子的血液浓度。
比较采用配对t检验。Kaplan-Meier生存分析评估一些测量值和无进展生存率或总生存率之间的相关性。
使用卡方检验评估部分缓解或疾病稳定组以及疾病进展组患者之间的Ktrans差异。这个试验是由国家食品药品监督管理局批准(批准号:s20050088)和中国国家食品药品监督管理局。审判是中国临床试验注册中心注册,编号chictr-ctr-09000569。书面知情同意和伦理批准。
此项研究一共招募了33例患者(年龄52岁-70岁,15名男性、18名女性),其中对28例进行了评估(治疗组20人,对照组8人)。五例患者排除:治疗组2例及对照组1例使用了粒细胞巨噬细胞集落刺激因子;对照组2例拒绝治疗。客观反应率较高(30% vs 0%;P<0.00001),平均总生存期较长(21.44个月 vs 7.71个月;P=0.008),使用重组人血管内皮抑素治疗组的毛细血管通透性降低(使用Ktrans评估)较比对照组高。治疗组疾病控制率为80%,对照组为75%(P=0.07)。
研究结果表明,使用重组人血管内皮抑制素与长春瑞滨-顺铂联合治疗增加非小细胞肺癌骨转移患者的治疗反应。使用动态增强MRI定量分析可用于评估治疗反应,并预测抗血管生成治疗后骨转移患者的生存率。
原始出处:
Zhang R, Wang ZY, Li YH, Lu YH, Wang S, Yu WX, Zhao H. Dynamic contrast-enhanced MRI to predict response to vinorelbine-cisplatin alone or with rh-endostatin in patients with non-small cell lung cancer and bone metastases: a randomised, double-blind, placebo-controlled trial. Lancet. 2016 Oct;388 Suppl 1:S95. doi: 10.1016/S0140-6736(16)32022-0.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#动态增强MRI#
87
#非小细胞#
85
#Lancet#
76
好文章,很好的的idea,受益匪浅。
130
关键在于有创新
127
谢谢分享!!!!!
96