Dig Dis Sci:肠溶布地奈德可用于治疗无反应的乳糜泻患者
2021-06-28 MedSci原创 MedSci原创
乳糜泻指对摄入的含麦麸食物产生过度免疫答的一种自身免疫性疾病,在美国和欧洲成人中发病率为0.2%-1%。现有研究证实,乳糜泻患病率呈上升趋势。20世纪80年代
乳糜泻指对摄入的含麦麸食物产生过度免疫答的一种自身免疫性疾病,在美国和欧洲成人中发病率为0.2%-1%。现有研究证实,乳糜泻患病率呈上升趋势。20世纪80年代以前,乳糜泻被认为是一种罕见疾病,其典型的临床表现为幼年时期营养吸收障碍、体重减轻、慢性腹泻或生长发育受限,而今乳糜泻已为常见疾病,并会在四、五十岁时出现非典型症状,如肠易激,腹痛,贫血等。

无反应性乳糜泻是指不进食含麸食物依然会出现上述症状的乳糜泻患者。本项研究旨在探究布地奈德可用于治疗难治性腹腔疾病 (RCD) 和腹腔危象以及具有绒毛萎缩 (VA) 的无反应性乳糜泻 (NRCD) 的临床和组织学反应的有效性。
研究人员对患有NRCD 和 VA 成人病例进行布地奈德处方的筛查和统计比较。评估了临床变量和粘膜恢复情况(即治疗后 1 年内的正常绒毛结构)。本项研究总共包括 42 例病例 [77% 女性,中位年龄 45.0 (IQR 28.3–60.0) 岁]。最常见的症状是腹泻 (64%) 和腹痛 (62%)。布地奈德起始剂量为 9 mg (83%),中位持续时间为 16.0 周(IQR 6.8-25.0 周)。总共有 57% 的患者表现出临床反应,临床效果与腹泻呈正相关(OR 6.08 95% CI 1.04–35.47),与疲劳呈负相关(OR 0.18 95% CI 0.03–0.98)。在布地奈德之前接受营养师咨询的患者的临床反应更高(n = 29, 70 vs. 23%,p < 0.01)。11名患者在随访进行十二指肠活检观察到粘膜结构的恢复。临床反应和粘膜恢复之间没有关联,79%的临床反应者有症状复发。RCD (48%) 和慢性麸质暴露 (24%) 是 NRCD 复发的主要病因。
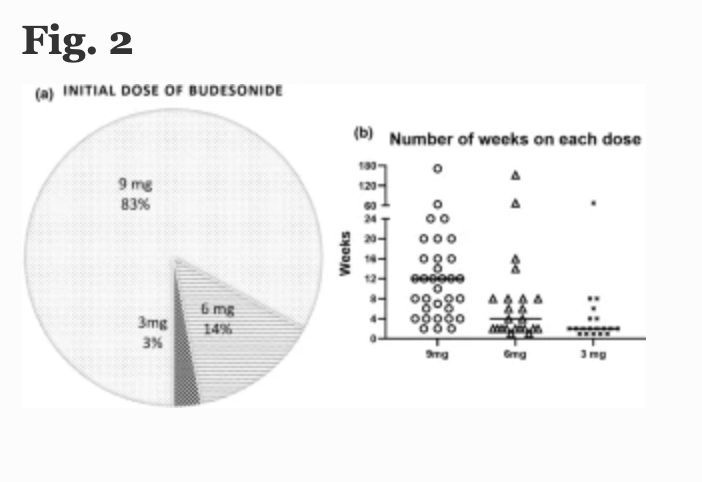
图:无反应乳糜泻的占比
本项研究证实布地奈德可能有效诱导以腹泻和 VA 为表现的 NRCD 的临床反应,但在逐渐减量后临床复发和黏膜恢复不足是常见的。
原始出处:
Amelie Therrien.et al. Enteric-Release Budesonide May Be Useful in the Management of Non-Responsive Celiac Disease. Digestive Diseases and Sciences.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Dis#
50
#布地奈德##乳糜泻#
149
学习好文
86
好
93
号
90