World J Pediatr:搬迁与环境清洁对降低NICU医疗保健相关感染发病率的影响
2018-03-19 检索与翻译:邵晓丹 审核:徐虹 SIFIC感染官微
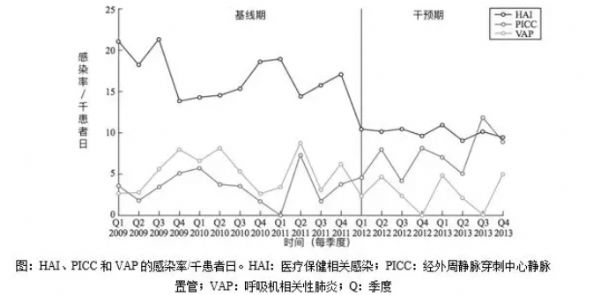
HAIs一直是新生儿重症监护病房(NICU)中新生儿发病和死亡的主要原因。尽管HAIs在入院患者中频繁发生,其中约30%可以通过特定的控制措施进行有效预防。由于NICU中危重新生儿的免疫系统不成熟,且接受了大量侵入性诊疗操作,罹患HAIs的风险大大增加。因此,在NICU对HAIs进行有效控制是至关重要的。


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#DIA#
40
#PE#
37
#发病率#
47
#医疗保健#
34
#NICU#
42
学习
59
学习了.谢谢分享.
59