女性滴虫病的治疗:Solosec®(secnidazole)的III期临床取得积极结果
2020-05-04 Allan MedSci原创
Lupin制药公司今天公布了其关键III期临床试验的顶线结果,该试验评估了单剂量Solosec®(secnidazole)治疗女性滴虫病的有效性和安全性。
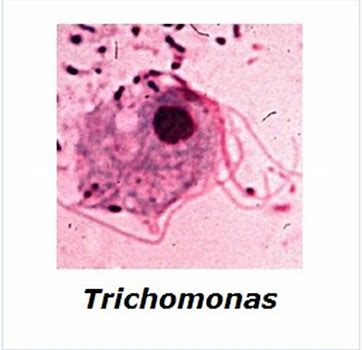
Lupin制药公司今天公布了其关键III期临床试验的顶线结果,该试验评估了单剂量Solosec®(secnidazole)治疗女性滴虫病的有效性和安全性。滴虫病是美国最常见的非病毒性可治愈性感染(STI)。该试验证明,与安慰剂相比,服用Solosec®的患者具有显著更高的缓解率和微生物学治愈率。根据这些数据,Lupin计划在2020年下半年向美国FDA提交Solotric®治疗滴虫病的补充新药申请(sNDA)。此前,Solosec®已获得FDA的批准,用以治疗成年女性细菌性阴道炎(BV)。
就微生物学治愈率而言,Solsec®(secnidazole)组为92.2%(59/64)和安慰剂组为1.5%(1/67)(p <0.001)。在Per-Protocol人群中,Solsec®(secnidazole)组的治愈率为94.9%(56/59),而安慰剂组的治愈率为1.7%(1/60)(p <0.001)。患者对Solsec®(secnidazole)的耐受性良好,最常见的不良反应是外阴阴道念珠菌病(2.7%)和恶心(2.7%),没有观察到严重的不良反应事件。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#I期临床#
55
#III#
69
#AZ#
52
#II期临床#
49
#III期#
55