NEJM:我国学者里程碑式研究,老年高血压患者强化降压确实更佳!
2021-09-01 MedSci原创 MedSci原创
将收缩压降至130 mmHg以下可为中国老年高血压患者带来心血管获益。
弗雷明汉(Framingham)心脏研究和其他研究表明,收缩期高血压作为心血管结局的预测因素,其重要性实际上超过舒张期高血压,因此有人呼吁“不再关注舒张压”。因此美国心脏病学会/美国心脏学会(ACC/AHA)风险估计工具在确定心血管风险时也未考虑舒张压。
然而,去年发表在《新英格兰医学杂志》(NEJM)杂志上的一项重磅研究则为舒张压进行了“正名”。研究对超过100万人、3600万次的血压测量数据显示,“上压”、“下压”都是心梗或中风发作风险的独立预测因素。2018年欧洲心脏病学会(ESC)高血压指南也建议所有风险水平患者的最佳舒张压目标为70至80 mmHg。
随后,今年5月NEJM再次发表了具有里程碑意义的高血压对心血管疾病影响(SPRINT研究的后续数据,证实,积极的血压管理--将收缩压降低到120mmHg以下--与将收缩压降低到140mmHg以下相比,大大降低了心脏病、中风和这些疾病的死亡风险,以及所有原因导致的死亡。
然而,对于老年高血压患者,尽管既往多项大型试验表明,强化降压有益心血管结局,但合适的收缩压目标尚不清晰,国际上现有指南推荐也不一致。尤其是没有适合适用于我国老年高血压患者治疗的目标收缩压。
为了对该问题进行进一步研究,来自我国国家心血管病中心、中国医学科学院阜外医院的心血管专家开展了一项名为STEP的研究,旨在使我国老年高血压患者实现更多的心脑获益。近期,相关结果发表在NEJM杂志上。
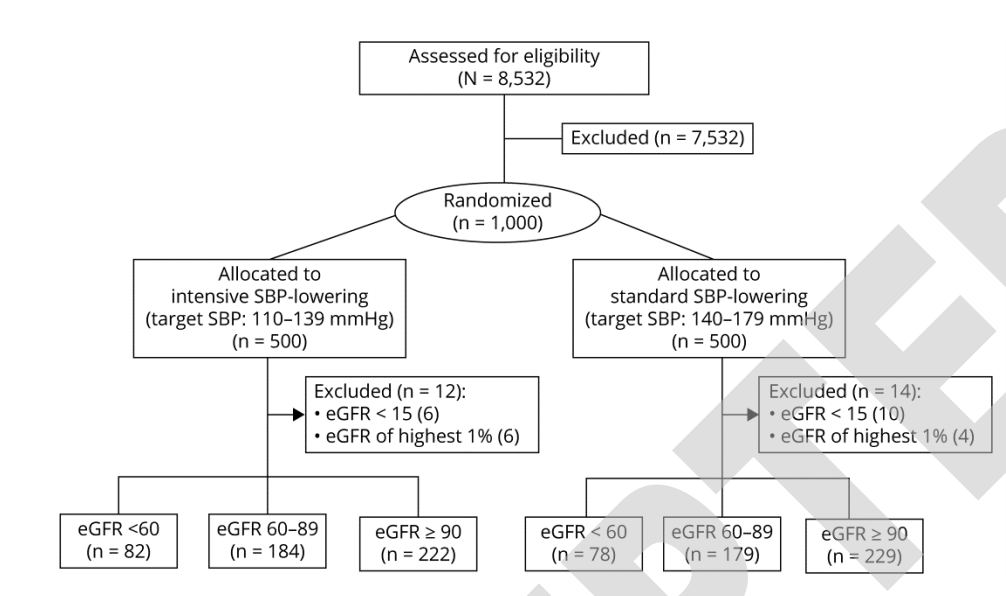
在这项多中心的随机对照试验中,研究人员将60至80岁的中国高血压患者分配到110-130mmHg的收缩压目标(强化治疗)或130-150mmHg的目标(标准治疗)。主要结果是中风、急性冠状动脉综合征(急性心肌梗死和不稳定心绞痛住院)、急性失代偿性心力衰竭、冠状动脉血运重建、心房颤动或心血管原因导致的死亡的综合发病率。
在经过筛选的9624名患者中,有8511人参加了该试验;4243人被随机分配到强化治疗组,4268人被分配到标准治疗组。在1年的随访中,强化治疗组的平均收缩压为127.5mmHg,标准治疗组为135.3mmHg。两组的舒张压分别为76.4 mmHg与79.2 mmHg。
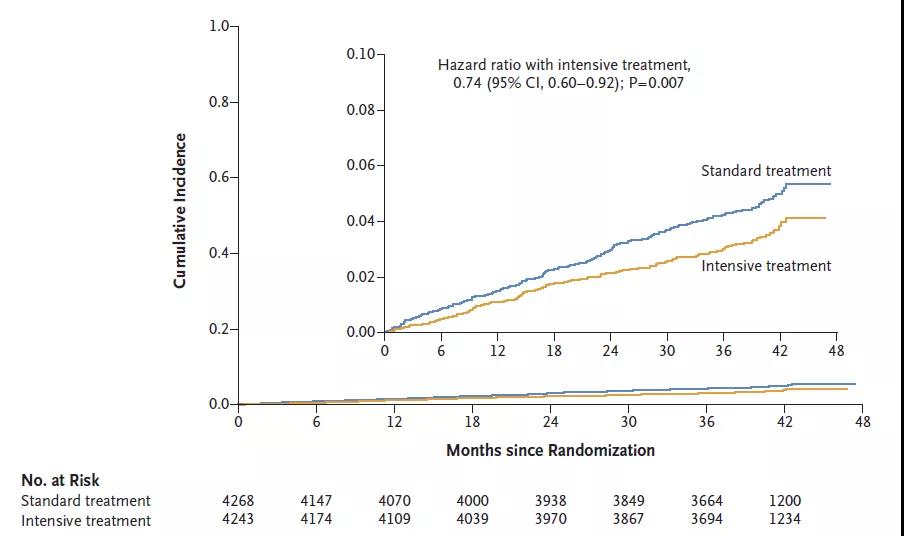
强化降压治疗组与标准降压治疗组的主要结局事件风险
在3.34年的中位随访期间,强化治疗组有147名患者(3.5%)发生了主要结果事件,而标准治疗组有196名患者(4.6%),强化组风险降低26%(HR=0.74;95%CI:0.60-0.92)。主要结果中的大多数单个组成部分的结果也有利于强化治疗:中风的危险降低33%(HR=0.67;95%CI,0.47-0.97),急性冠状动脉综合征降低33%(HR=0.67;95%CI,0.47-0. 94),急性失代偿性心力衰竭降低73%(HR=0.27,95%CI,0.08-0.98)。
然而,冠状动脉血运重建(HR=0.69, 95%CI,0.40-1.18)、心房颤动(HR=0.96;95%CI,0.55-1.68),和心血管原因导致的死亡(HR=0.72;95%CI,0.39-1.32)。此外,除了低血压的发生率在强化治疗组更高之外,两组之间的安全性和肾脏结果没有显著差异。
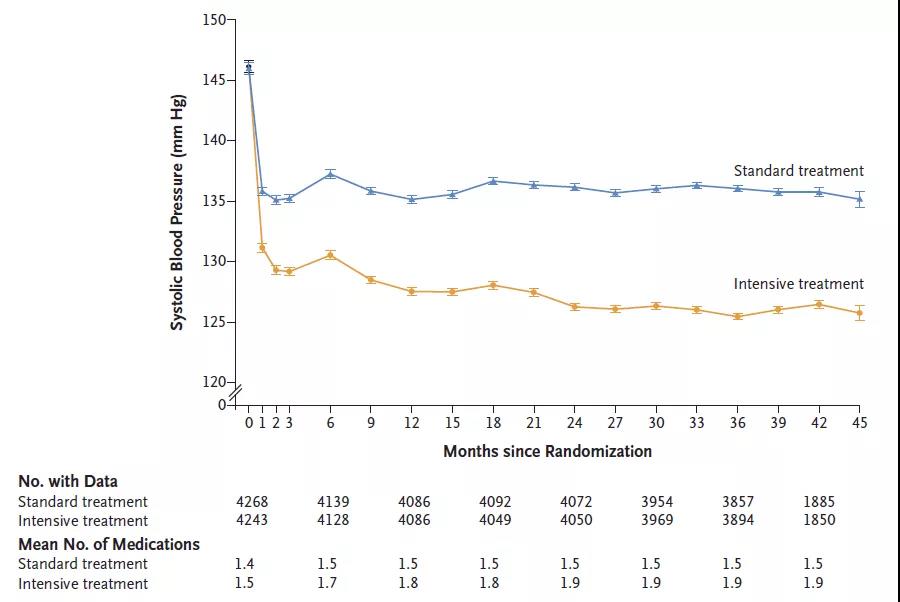
强化降压治疗组与标准降压治疗组的血压变化
综上,STEP大型试验提供了重要证据,表明将收缩压降至130 mmHg以下可为中国老年高血压患者带来心血管获益。
参考文献:
Trial of Intensive Blood-Pressure Control in Older Patients with Hypertension. August 30, 2021. DOI: 10.1056/NEJMoa2111437
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#里程碑式研究#
84
#里程碑#
83
#我国学者#
72
#降压#
77
#强化降压#
138
#高血压患者#
81
#老年高血压#
118
强
94
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
75