Lancet oncol:AML移植后采用索拉菲尼维持治疗的疗效和耐受性
2020-08-11 MedSci原创 MedSci原创
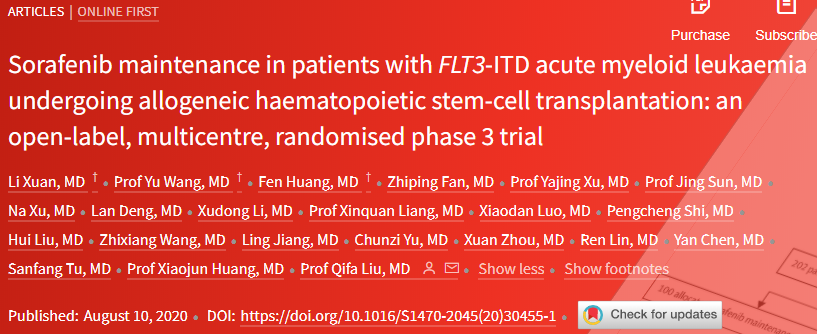
索拉非尼维持治疗或可减少FLT3-ITD急性髓系白血病患者异基因造血干细胞移植后的复发。南方医科大刘启发主任率领团队开展了一项3期试验,评估这类患者采用索拉菲尼维持治疗的疗效和安全性。
回顾性研究结果表明,索拉非尼维持治疗或可减少携带FLT3内部串联重复(FLT3-ITD)的急性髓系白血病患者异基因造血干细胞移植后的复发。
南方医科大学血液科刘启发主任率领团队开展了一项开放性的随机3期试验,评估这类患者异基因造血干细胞移植后索拉菲尼维持治疗的疗效和耐受性。主要终点是1年累计复发率。
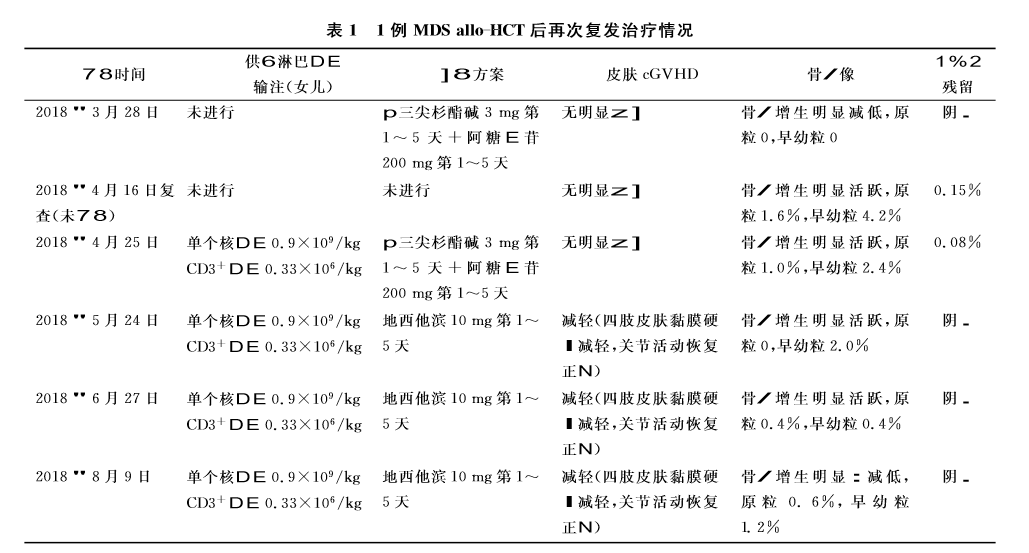
该试验招募18-60岁的携带FLT3-ITD的计划进行异基因造血干细胞移植的急性髓系白血病患者,且要求ECOG表现状态0-2分,在移植前后获得完全缓解,并在移植后60天内获得血液学恢复。
2015年6月20日-2018年7月21日,共招募了202位患者,随机分至索拉菲尼维持组(100人,索拉菲尼 400 mg,口服,2/日)或对照组(102人)。
移植后中位随访21.3个月。索拉菲尼组和对照组的1年累计复发率分别是7.0%和24.5%(风险比[HR]0.25)。在移植后的210天内,最常见的3/4级不良反应有感染(24% vs 24%)、急性移植物抗宿主病(GVHD 23% vs 21%)、慢性GVHD(18% vs 17%)和血液毒性(15% vs 7%)。无治疗相关死亡。
移植后索拉菲尼维持治疗可减少FLT3-ITD型急性髓系白血病的复发,而且耐受性良好。该治疗方案或可成为FLT3-ITD急性髓系白血病患者的新治疗选择。
原始出处:
Li Xuan,et al. Sorafenib maintenance in patients with FLT3-ITD acute myeloid leukaemia undergoing allogeneic haematopoietic stem-cell transplantation: an open-label, multicentre, randomised phase 3 trial. The Lancet Oncology. August 10,2020.https://doi.org/10.1016/S1470-2045(20)30455-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Lancet#
84
#Oncol#
88
#索拉菲尼#
78
#耐受性#
67
谢谢梅斯提供这么好的信息,学到很多
116
顶刊就是不一样,质量很高,内容精彩!学到很多
75
谢谢梅斯分享这么多精彩信息
93