AJRCCM:口服曲前列丁尼联合治疗肺动脉高压,一项双盲、安慰剂对照的临床试验
2021-11-02 刘少飞 MedSci原创
口服曲前列环素改善了初治肺动脉高压 (PAH) 患者的运动能力,这项多中心、随机、双盲安慰剂对照试验表明,对于最近开始口服 PAH 单药治疗的参与者,开始口服曲前列环素可降低临床恶化事件的风险。

肺动脉高压 (PAH) 是一种罕见但进行性且通常致命的肺血管疾病。在过去的 20 年中,治疗选择有了很大的扩展,两项序贯联合治疗的事件驱动研究已经确定了内皮素受体拮抗剂 (ERA) 马昔腾坦和前列环素受体激动剂司来帕格的持久益处。依前列醇是前列环素受体的内源性激动剂,对 PAH 非常有效,但作用时间短,需要持续静脉输注。因此,司来帕格作为一种长效且可口服的选择性前列环素 IP 受体激动剂是治疗选择的重要补充。口服缓释曲前列环素二醇胺片在未接受过治疗的 PAH 患者中每天服用两次可提高运动能力。每天给药 3 次的口服曲前列环素具有更好的药代动力学特征,允许参与者达到更高的每日总剂量,并在一组精心挑选的 PAH 参与者中替代了肠外曲前列环素。因此,FREEDOM-EV 研究假设,对于最近开始口服 PAH 单药治疗的患者,口服曲前列环素联合治疗将降低临床恶化事件的风险。
研究设计:
FREEDOM-EV 试验是一项多中心、随机、双盲、安慰剂对照、事件驱动的研究。 来自 23 个国家的 152 个中心的研究人员在 2012 年 6 月至 2018 年 6 月期间进行了这项研究。
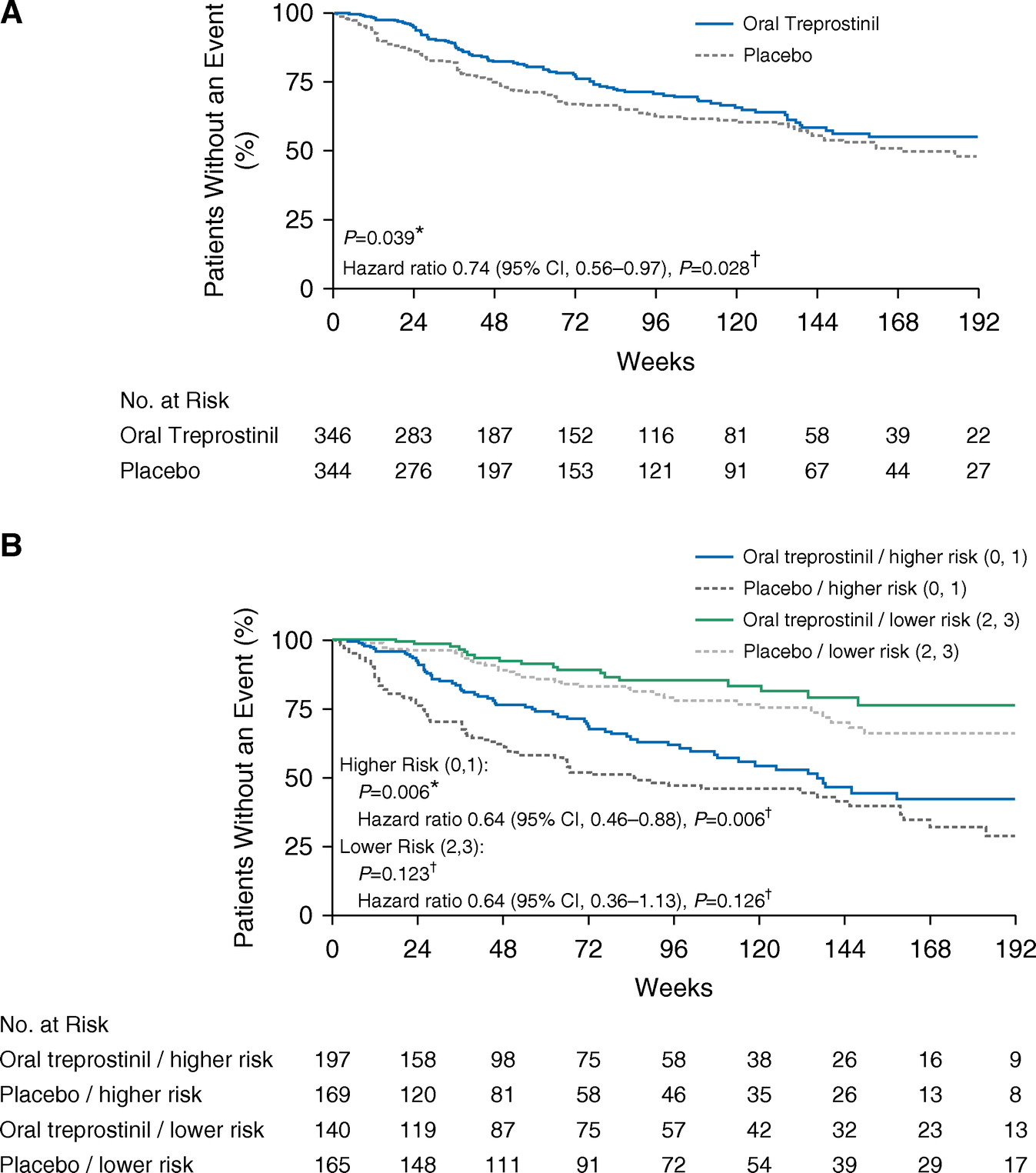
研究入选了690 名参与者随机分配到口服曲前列素(346 名参与者)或安慰剂(344 名参与者)治疗组(图下)。

总体而言,与 124 名 (36%) 安慰剂参与者相比,口服曲前列环素组的 90 名参与者 (26%) 经历了经裁定的临床恶化事件。 Kaplan-Meier 对判定临床恶化事件的时间的估计表明在第 24 周之前进行了分组(图下A,P = 0.039);根据背景治疗和基线 6MWD 作为连续变量调整的风险比为 0.74(95% CI,0.56–0.97;P = 0.028)。当将基线 6MWD 作为分类变量(断点≤350 m)进行调整时,风险比为 0.75(95% CI,0.57–0.99;P = 0.040)。口服曲前列素组至临床恶化的中位时间为 46 周,安慰剂组为 37 周。治疗引起的临床恶化差异是由口服曲前列环素组疾病进展发生率降低所致(风险比,0.39;95% CI,0.23–0.66;P < 0.001)。死亡和住院是平衡的。基于年龄、性别、基线 6MWD、WHO 功能分类、PAH 病因、地理区域和口服 PAH 治疗背景的主要终点的亚组分析未显示亚组和治疗之间有任何显着的相互作用。
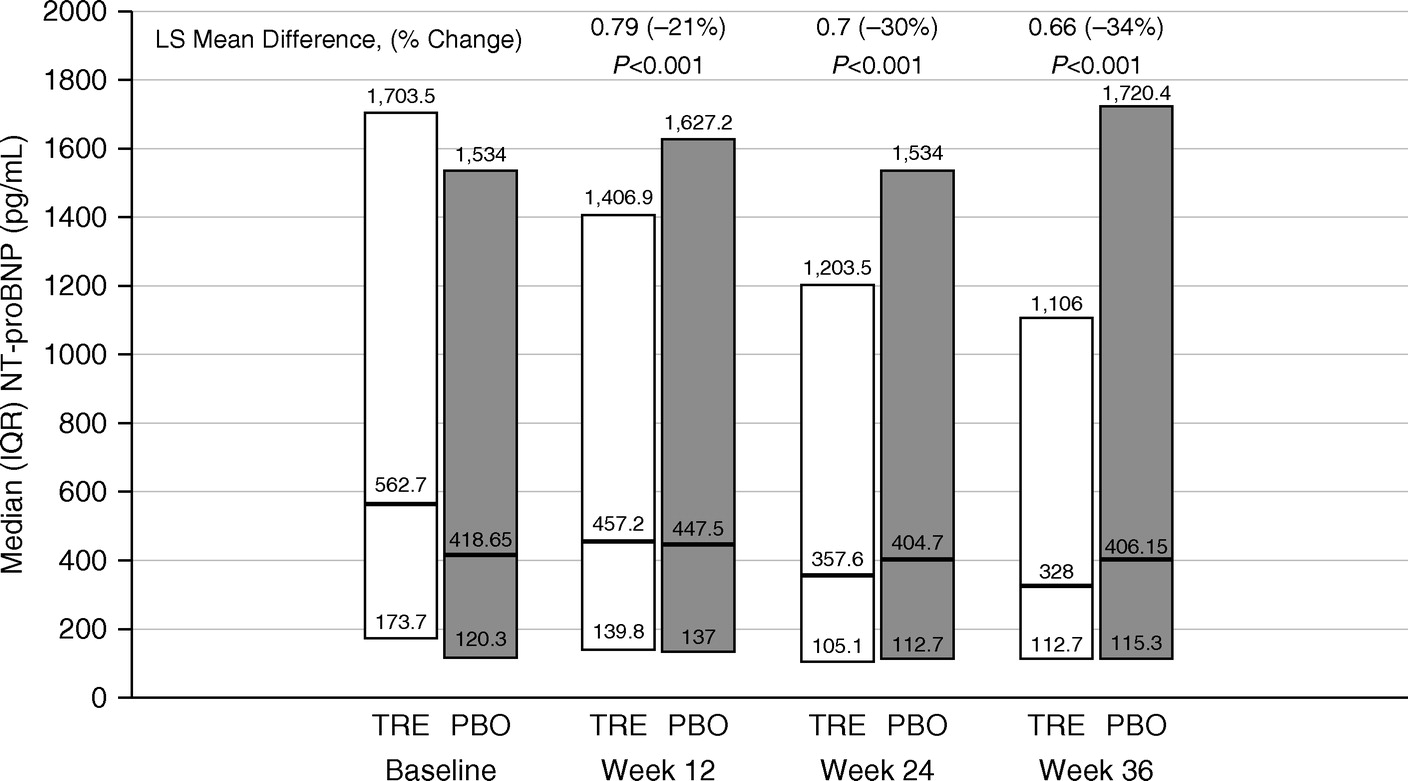
从第 12 周开始,口服曲前列环素组的血浆 NT-proBNP 水平下降(图下)。
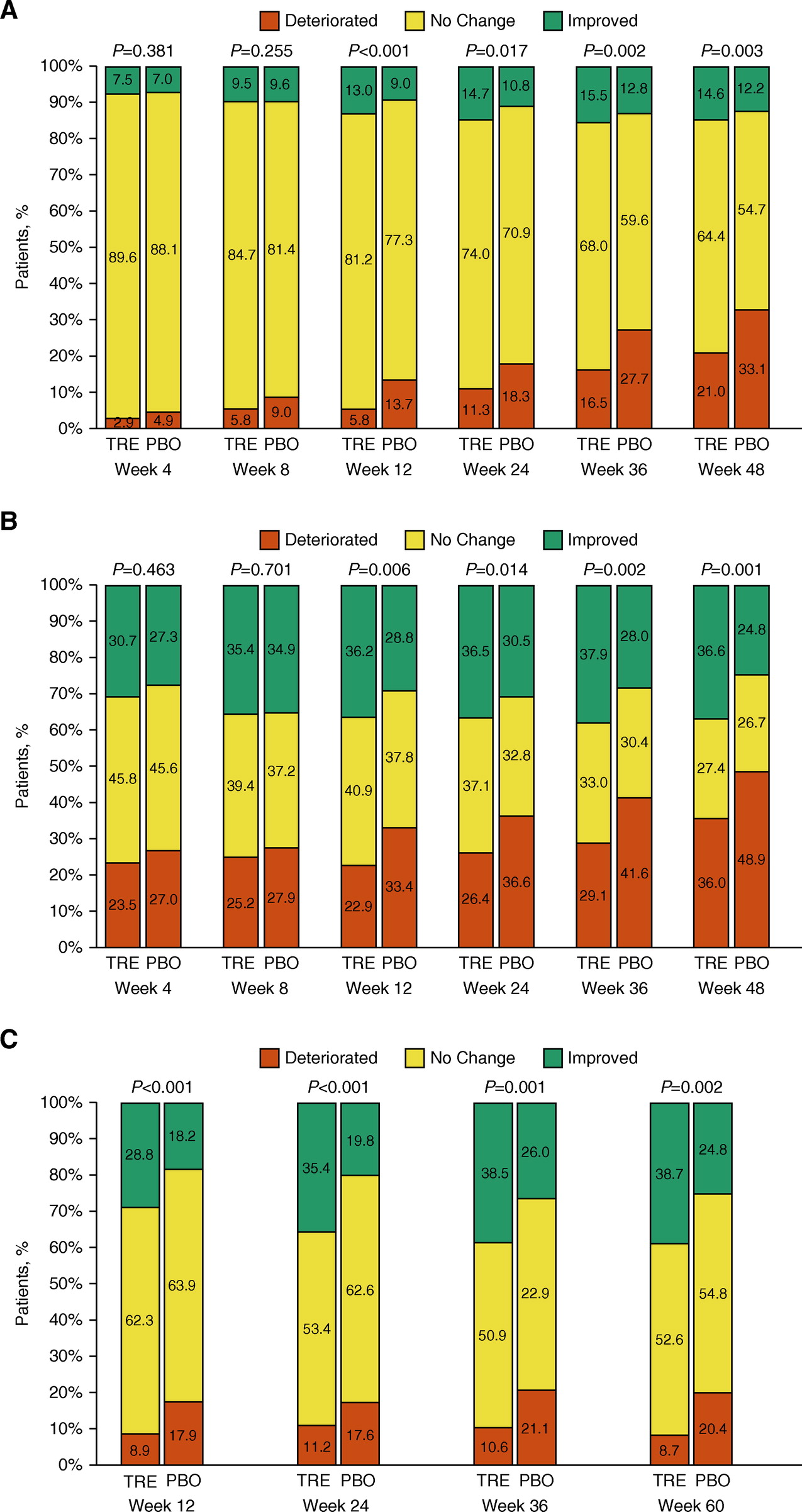
与安慰剂组相比,口服曲前列环素组参与者在第 12 周至第 48 周的所有访问中的 WHO 功能等级显着改善。
该研究有一定的局限性。前列环素类药物的典型不良反应很常见,18.8% 的停药率高于先前对司来帕格的研究 (14.3%)。可以想象,一些因不良事件而停止服用该药的口服曲前列素参与者后来可能会出现临床恶化,但我们在生成主要结果分析时使用了标准审查方法。该方案于 2013 年推出,当时序贯联合治疗成为标准,但初始联合治疗正变得越来越普遍。目前尚不清楚目前的结果是否可以推广到已经在接受两种批准疗法的临床实践中的患者。
总之,口服曲前列环素每天 3 次给药于一组相对均质的 PAH 参与者,这些参与者正在接受口服单一疗法,降低了由于疾病进展导致临床恶化的可能性。口服曲前列环素后血浆 NT-proBNP 水平显着下降,我们还观察到研究者评估的 WHO 功能等级和参与者报告的走廊行走后 Borg 呼吸困难评分有所改善。连续的、无创的风险评分测量似乎有助于记录治疗相关的益处,未来的结果研究应考虑预后评分,以平衡随机治疗组之间的基线风险状况。
文献出处:
White RJ, Jerjes-Sanchez C, Bohns Meyer GM, Pulido T, Sepulveda P, Wang KY, Grünig E, Hiremath S, Yu Z, Gangcheng Z, Yip WLJ, Zhang S, Khan A, Deng CQ, Grover R, Tapson VF; FREEDOM-EV Investigators. Combination Therapy with Oral Treprostinil for Pulmonary Arterial Hypertension. A Double-Blind Placebo-controlled Clinical Trial. Am J Respir Crit Care Med. 2020 Mar 15;201(6):707-717. doi: 10.1164/rccm.201908-1640OC. PMID: 31765604; PMCID: PMC7068822.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#RCC#
108
#动脉高压#
83
#对照#
98
#安慰剂#
110
#联合治疗#
72
#双盲#
115
#安慰剂对照#
103