AJRCCM:在肺动脉高压中BMP9和BMP10基因突变及其水平的特征
2021-11-02 刘少飞 MedSci原创
人类遗传学研究揭示了对 PAH 病理生物学的重要见解。该研究试图根据生化表征和患者 BMP9 血浆水平的测量,确定最近发现的 GDF2 中的新杂合突变是否会导致 BMP9 功能丧失。

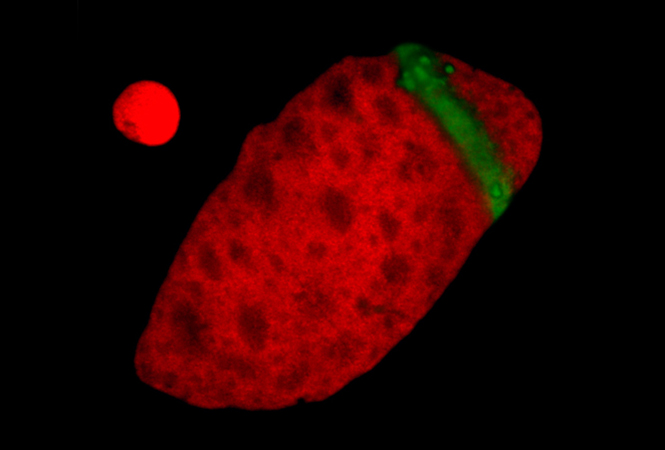
肺动脉高压 (PAH) 是一种罕见但重要的限制生命的疾病,通常表现为运动时无法解释的呼吸困难。肺病理的特征在于由血管壁中的内皮细胞、平滑肌细胞和成纤维细胞的增殖导致的小肺动脉变窄和闭塞。由此导致的肺血管阻力升高导致严重的 PAH。压力超负荷的右心室最初通过肥大作出反应,但最终扩张并失败。尽管存在现有疗法,但平均无移植 3 年生存率仍仅为60%至70%,需要在对病理生物学更透彻的了解的基础上寻找更有效的治疗方法。最近,在肺动脉高压 (PAH) 患者中发现了 GDF2 中罕见的杂合突变。 GDF2 编码循环 BMP(骨形态发生蛋白)9 型,它是 BMP2 受体的配体。体外表达错义 BMP9 突变蛋白,并评估对 BMP9 蛋白加工和分泌、内皮信号传导和功能活性的影响。 在具有 GDF2 变体的 PAH 患者和对照受试者中检测血浆 BMP9 和 BMP10 水平和活性。 还在更大的对照组(n = 120)和特发性多环芳烃患者(n = 260)中测量了水平。
研究目的:已在肺动脉高压 (PAH) 中鉴定出BMP9中的罕见突变。 尚不清楚在 PAH 中特异性识别的 BMP9 变体是否与那些不完全与 PAH 相关的变体具有不同的功能变化。确定了 GDF2 突变的功能影响,并检测特发性 PAH 患者的血浆 BMP9 和 BMP10 水平。
入选患者:对 1,048 名 PAH 患者进行了全基因组测序,并进行了病例对照罕见变异分析。
研究结果:
BMP9突变及BMP9突变体的特点;
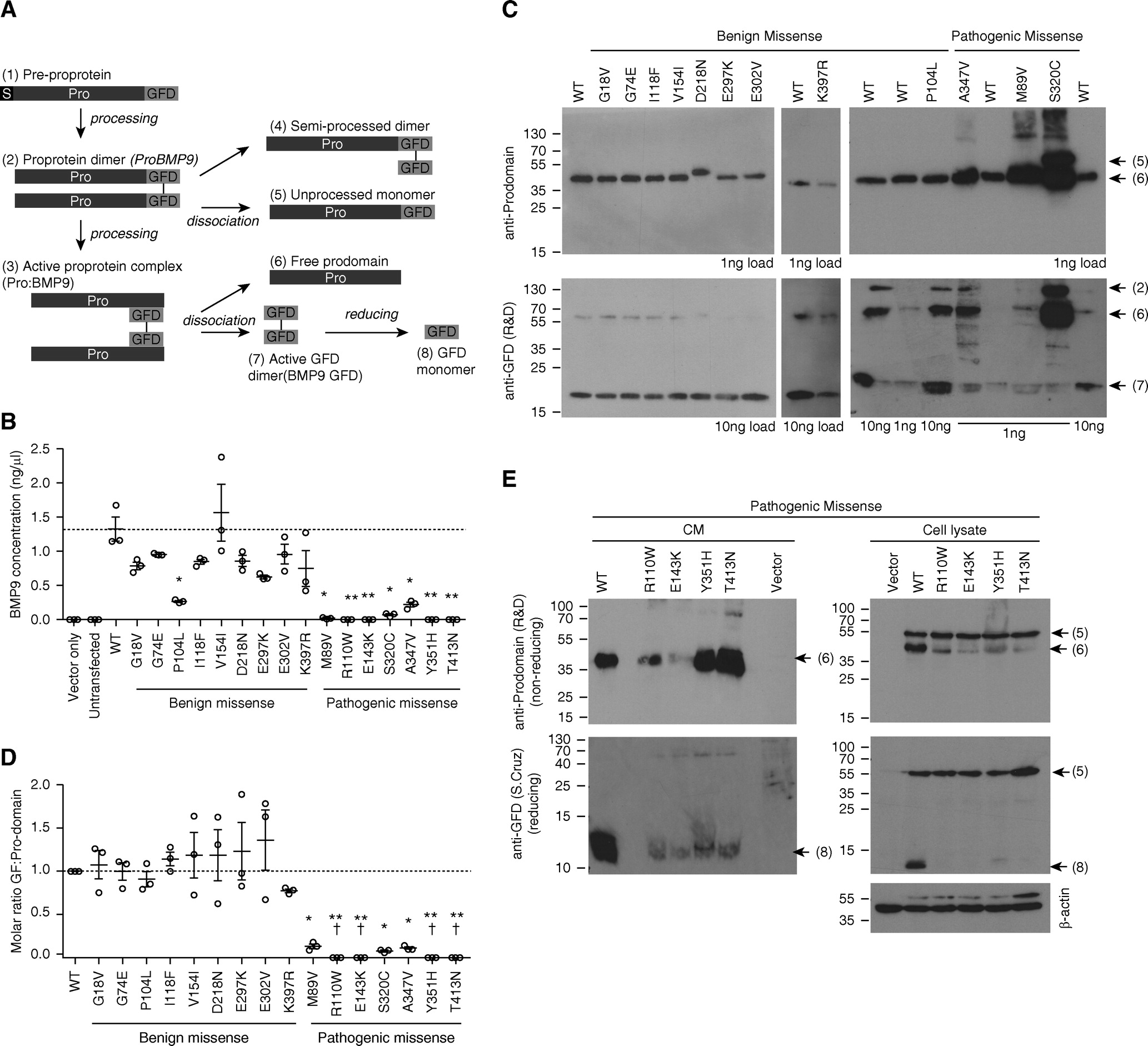
Pro:BMP9突变体中的活性丧失被预测具有致病性
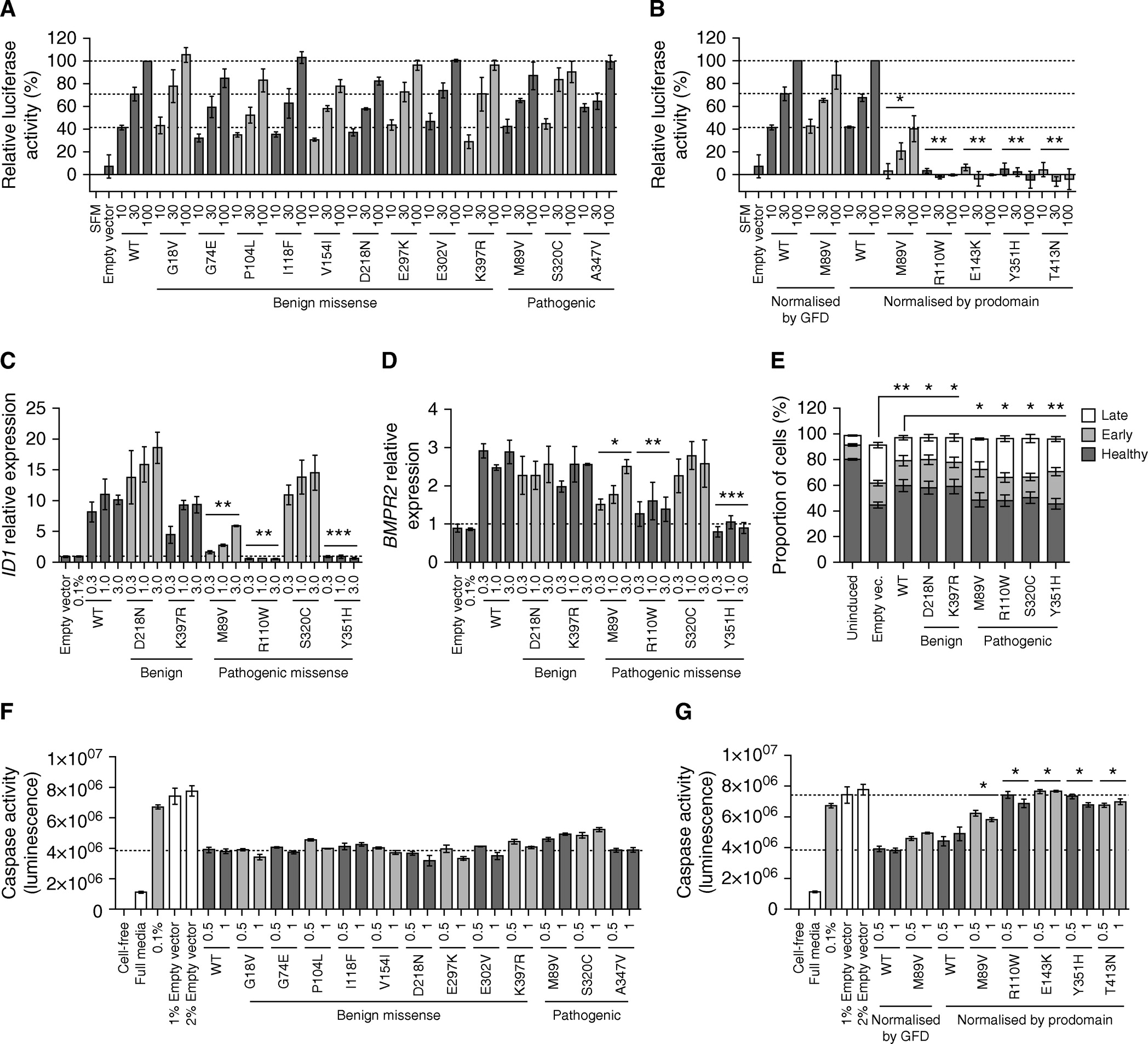
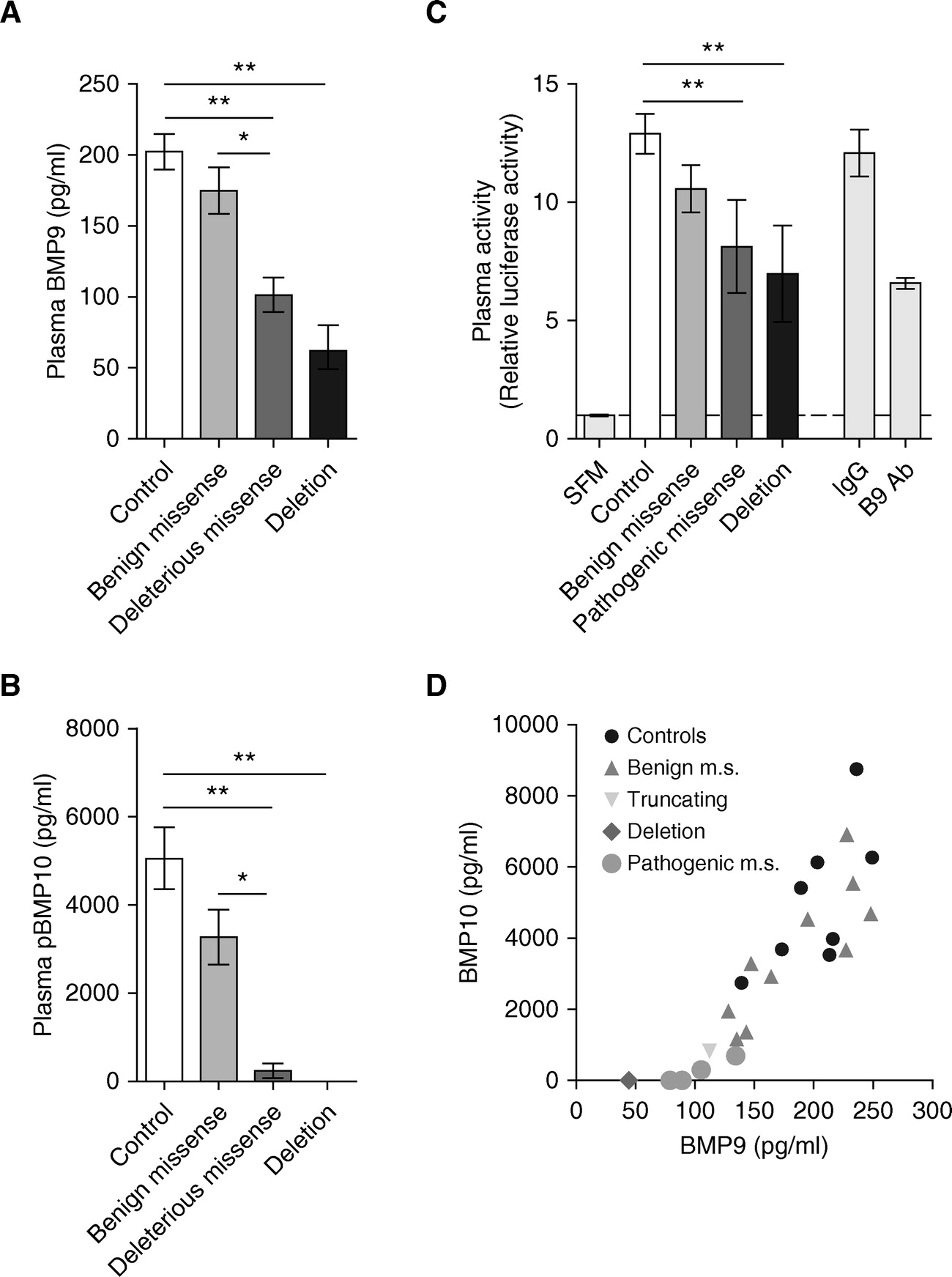
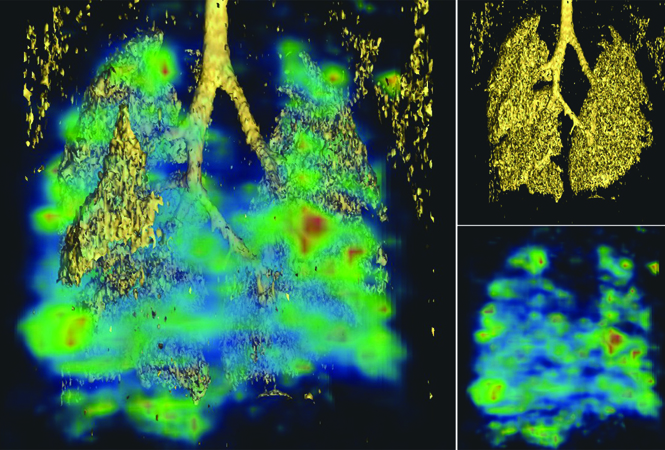
携带假定致病性 GDF2 等位基因的肺动脉高压患者失去活性 BMP9,使用经验证无交叉反应性、加标回收率和血浆测定稀释剂的 BMP9 ELISA 方案,该研究测量了患者的循环 BMP9 血浆水平和活性携带 GDF2 突变。
血浆 BMP9和 pBMP10 水平在肺动脉高压 (PAH) 中没有降低,但一部分 PAH 患者表现出血浆 BMP9 和 pBMP10 水平降低。该研究比较了 BMP9和 pBMP10三分位数之间的临床特征,并且还对配体浓度和临床参数之间的关系(连续变量)进行了相关分析。 在 PAH 患者中,BMP9 和 pBMP10 水平与通过 6 分钟步行测试测量的运动能力无关。 38 名患者可获得与采样时间同时期的血流动力学,但未显示与 BMP 有任何相关性。 值得注意的是,在 PAH 病例中,BMP9 和 pBMP10 水平与体重指数 (BMI) 呈负相关,但在对照受试者中则不然。
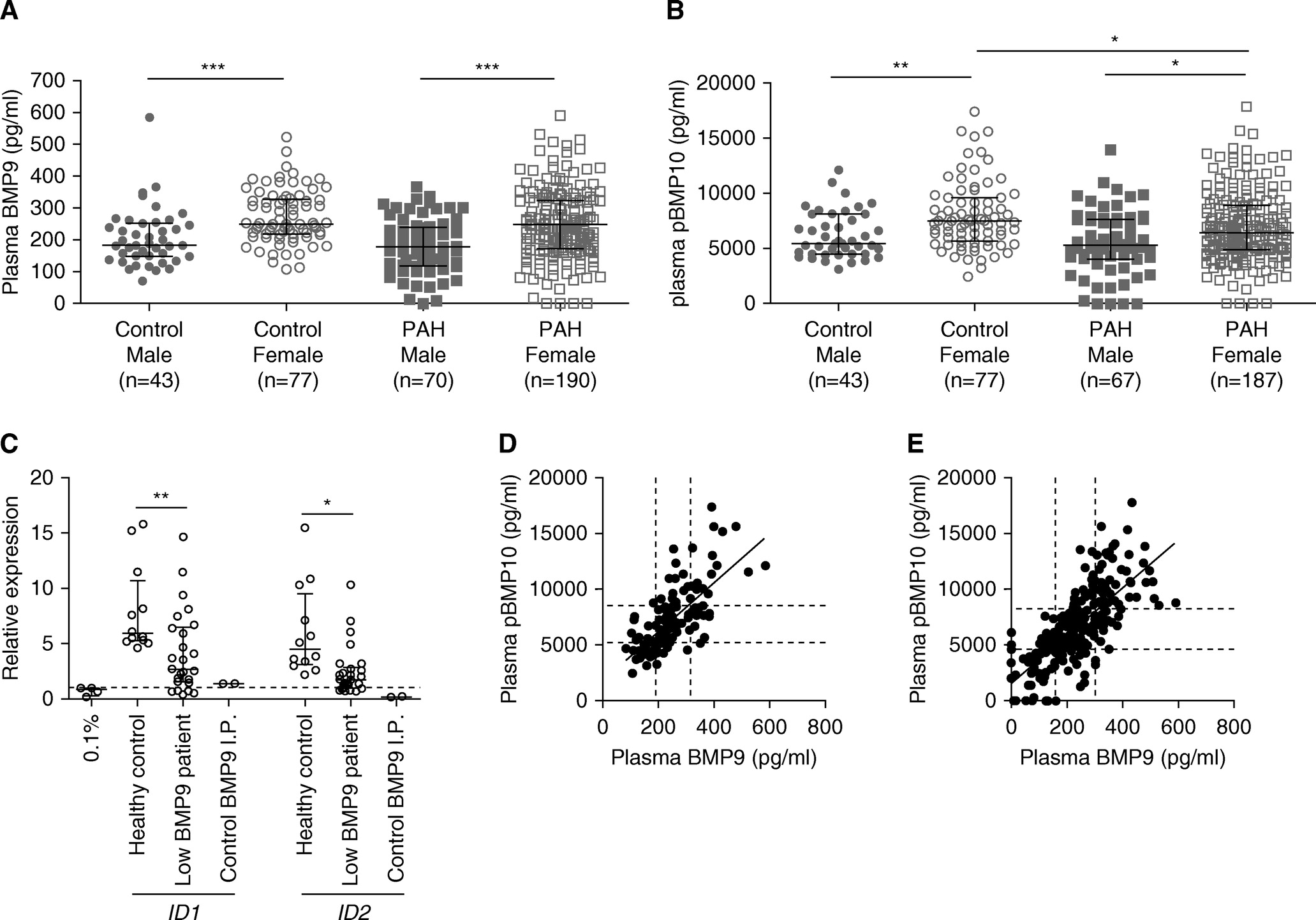
这项研究对欧洲大型 PAH 患者队列中发现的BMP9中罕见的潜在破坏性突变进行了详细的功能分析。 大多数突变导致成熟蛋白质的细胞加工改变和细胞分泌减少。 这些突变与这些个体中 BMP9 的循环水平降低和血浆 BMP9 活性降低有关。 这些发现支持了这些突变在 PAH 病理生物学中的因果作用,并为人类提供了强有力的证据,即 BMP9 水平和活性的降低促进了 PAH 的发展。 此外,两名BMP9基因座缺失患者的发现提供了新的遗传证据,支持 PAH 的因果作用。
文章出处:
Hodgson J. Characterization of GDF2 Mutations and Levels of BMP9 and BMP10 in Pulmonary Arterial Hypertension. Am J Respir Crit Care Med. 2020 Mar 1;201(5):575-585. doi: 10.1164/rccm.201906-1141OC. PMID: 31661308; PMCID: PMC7047445.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BMP#
138
#动脉高压#
115
#RCC#
127
学习
159
学习一下
150
动脉高压 (PAH) 是一种罕见但重要的限制生命的疾病
143