抑制microRNA-30a可减轻肺动脉高压的血管重构
2021-10-29 刘少飞 MedSci原创
过多和异位的肺动脉平滑肌细胞对肺动脉高压 (PAH) 中肺小动脉 (PA) 重塑的发病机制至关重要。抑制 miR-30a 可以通过 miR-30a/P53 信号通路改善实验性PAH。
肺动脉高压 (PAH) 是一种破坏性疾病,其特征是进行性肺小动脉 (PA) 重构,导致右心室 (RV) 后负荷增加并最终导致死亡。 近 20 年来,PAH 的治疗取得了长足的进步,尤其是随着靶向药物的应用。然而,目前这些治疗仅限于血管收缩,大约在 5% 的 PAH 患者中起作用,并且几乎不能逆转重塑血管。研究表明,SMCs 而不是内皮细胞 选择作为细胞来源建立新内膜以闭塞小动脉。因此,探索预防SMC重塑的新方法在治疗PAH中具有重要意义。
在该团队之前的研究中,发现 miR-30a 在体内急性心肌梗死(AMI)患者和动物的血清中以及体外缺氧刺激后培养的心肌细胞中显着升高,并通过抑制自噬使心脏功能恶化。同样,缺氧是 PAH 血管重塑的关键触发机制,并且 miR-30a 水平的变化也可能参与 PASMC 的重塑。 本研究重点关注缺氧后 PAH 患者、PAH 动物模型和 PASMC 中 miR-30a 的变化。 还通过 Su5416/缺氧诱导和野百合碱 (MCT) 诱导的 PAH 动物中 miR-30a 的遗传和药理学抑制来评估对 PA 和 RV 重塑的影响。 此外,使用 miR-30a 抑制剂的气管内液体滴注 (IT-L) 来探索一种新的 PAH 治疗递送策略。

研究设计:
研究首先发现了PAH患者、PAs和PASMCs缺氧后miR-30a升高;沉默 miR-30a 可减轻 Su5416/缺氧小鼠模型中的 RV 收缩压 (RVSP) 和 RV 肥大。
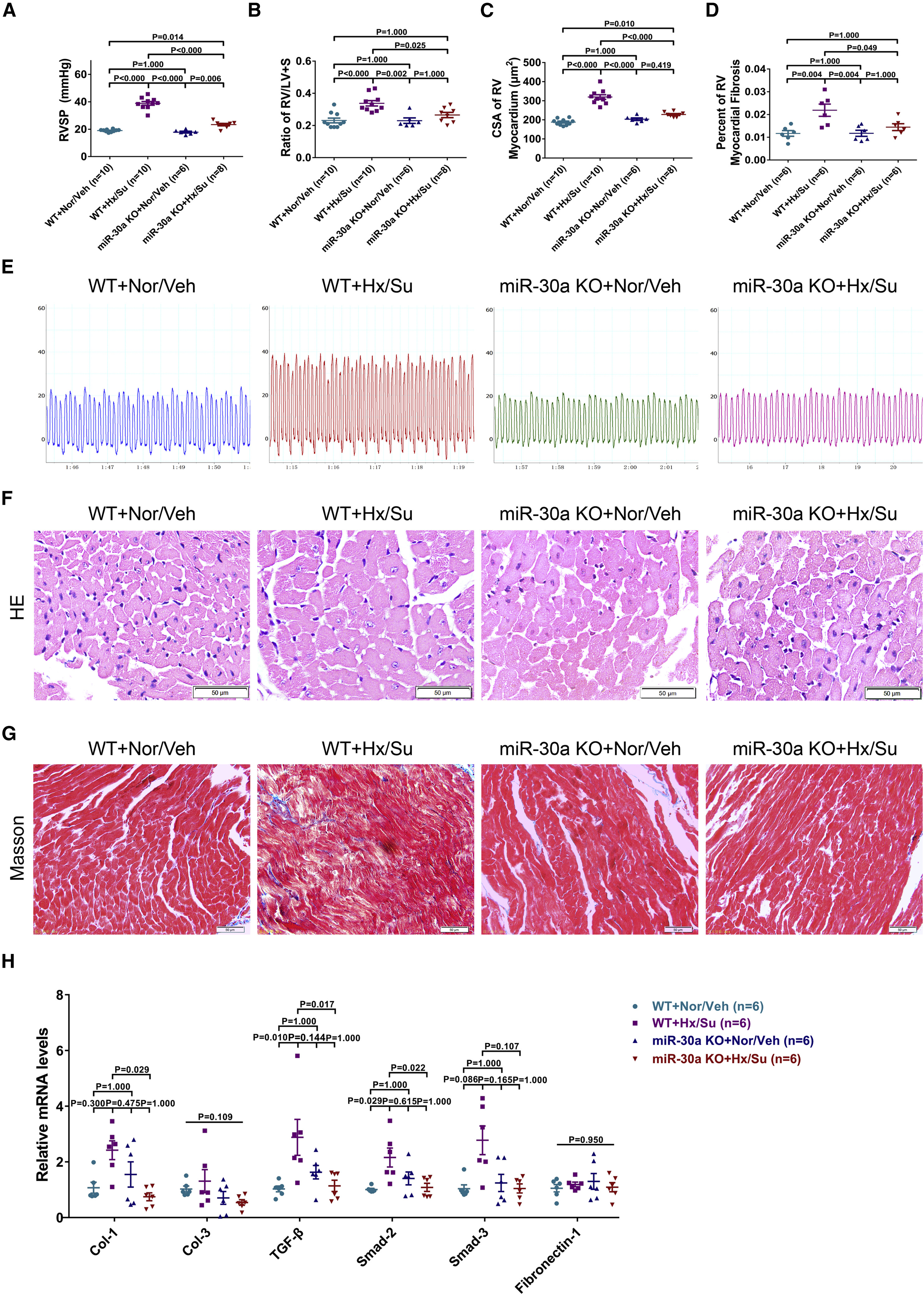
动物模型1:敲除 miR-30a 激活 PA 细胞凋亡以防止 Su5416/缺氧小鼠模型中的血管重构;
动物模型2:敲除 miR-30a 可增强 PA 的凋亡以逆转 MCT 小鼠模型中的血管重塑;同时,敲除 miR-30a 可减轻 MCT 小鼠模型中的 RVSP、RV 肥大和纤维化;
本研究首次确定了 miR-30a 在 PAH 中的作用,并通过抑制 miR-30a 来描述其治疗效果。 该研究观察到 miR-30a 在 PAH 患者的血清中以及在缺氧后 PAH 动物的 PA 和 PASMC 中的表达增加。 此外,发现 miR-30a 介导了 PASMC 中 P53 的下调。 在 Su5416/缺氧诱导和 MCT 诱导的 PAH 动物中,miR-30a 的基因缺失有效地逆转了 PA 重塑并增加了 RVSP 和 RV 肥大。 此外,IT-L 递送策略显示出高效率,可降低 miR-30a 水平并减轻 PAH 的疾病表型,同时抑制 P53 可以部分降低这些有益作用。
文章出处:
Ma W, Qiu Z, Bai Z, Dai Y, Li C, Chen X, Song X, Shi D, Zhou Y, Pan Y, Liao Y, Liao M, Zhou Z. Inhibition of microRNA-30a alleviates vascular remodeling in pulmonary arterial hypertension. Mol Ther Nucleic Acids. 2021 Sep 20;26:678-693. doi: 10.1016/j.omtn.2021.09.007. PMID: 34703652; PMCID: PMC8517099.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#动脉高压#
76
#血管重构#
83
#Micro#
61
#CRO#
66
#microRNA#
103