Eur Heart J:计算机断层扫描冠状动脉造影获得的血流储备分数在稳定型胸痛评估中的价值
2021-07-19 MedSci原创 MedSci原创
对于稳定型心绞痛患者进行选择性FFRCT获得CTCA的策略在成本或临床结局方面与标准临床处理途径没有显著差异,但确实减少了有创冠状动脉造影的使用程度。
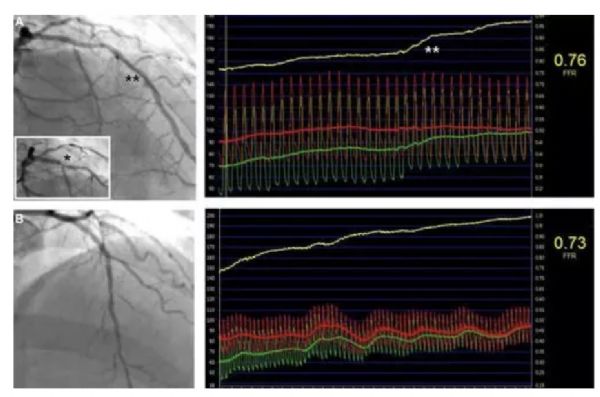
使用计算机断层扫描冠状动脉造影 (CTCA) 获得的血流储备分数 (FFRCT) 可确定冠状动脉疾病和血管特异性缺血。

近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员评估了基于FFRCT的评估策略与标准处理相比是否会改善经济和临床结局。
 总体而言,11个中心的1400名稳定型胸痛患者随机接受CTCA和选择性FFRCT实验组)或标准临床处理途径(标准组)。该研究的主要终点是9个月时的心脏总费用;次要终点是心绞痛状态、生活质量、主要不良心脑血管事件以及有创冠状动脉造影的使用情况。
总体而言,11个中心的1400名稳定型胸痛患者随机接受CTCA和选择性FFRCT实验组)或标准临床处理途径(标准组)。该研究的主要终点是9个月时的心脏总费用;次要终点是心绞痛状态、生活质量、主要不良心脑血管事件以及有创冠状动脉造影的使用情况。
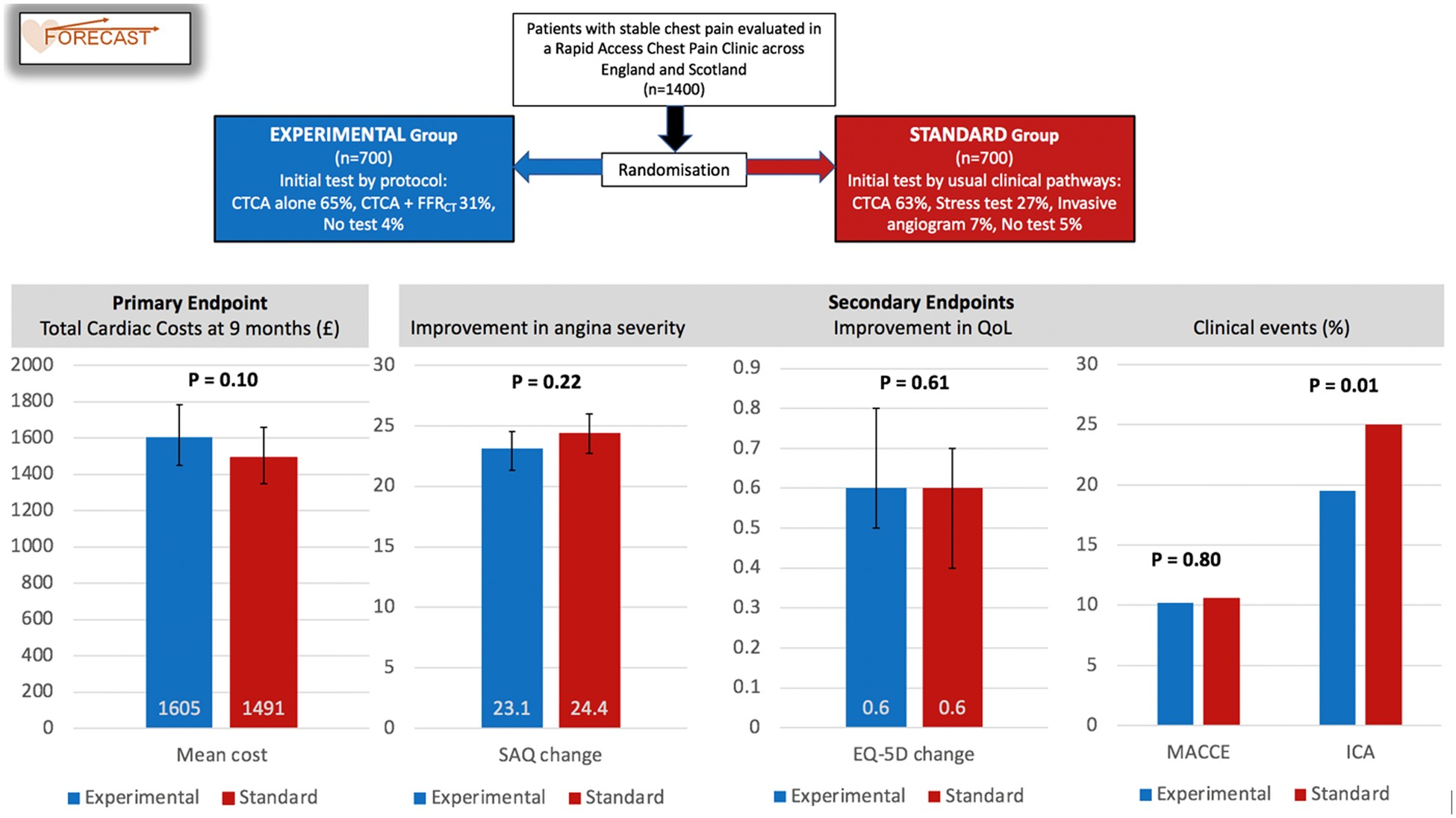 随机分组的患者在基线时相似。大多数患者进行了CTCA检查:标准组439例(63%)与实验组674例(96%),其中 254例(38%) 接受了FFRCT检查。实验组的平均心脏总费用高出114英镑(+8%),95%置信区间从-112(-8%)到+337(+23%),但差异不显著(P=0.10)。主要不良心脏和脑血管事件没有显著差异(实验组为10.2%,标准组为10.6%),并且两个组的心绞痛和生活质量在随访期间的改善程度相似。实验组有创血管造影显著减少(19% vs. 25%,P=0.01)。
随机分组的患者在基线时相似。大多数患者进行了CTCA检查:标准组439例(63%)与实验组674例(96%),其中 254例(38%) 接受了FFRCT检查。实验组的平均心脏总费用高出114英镑(+8%),95%置信区间从-112(-8%)到+337(+23%),但差异不显著(P=0.10)。主要不良心脏和脑血管事件没有显著差异(实验组为10.2%,标准组为10.6%),并且两个组的心绞痛和生活质量在随访期间的改善程度相似。实验组有创血管造影显著减少(19% vs. 25%,P=0.01)。
由此可见,对于稳定型心绞痛患者进行选择性FFRCT获得CTCA的策略在成本或临床结局方面与标准临床处理途径没有显著差异,但确实减少了有创冠状动脉造影的使用程度。
原始出处:
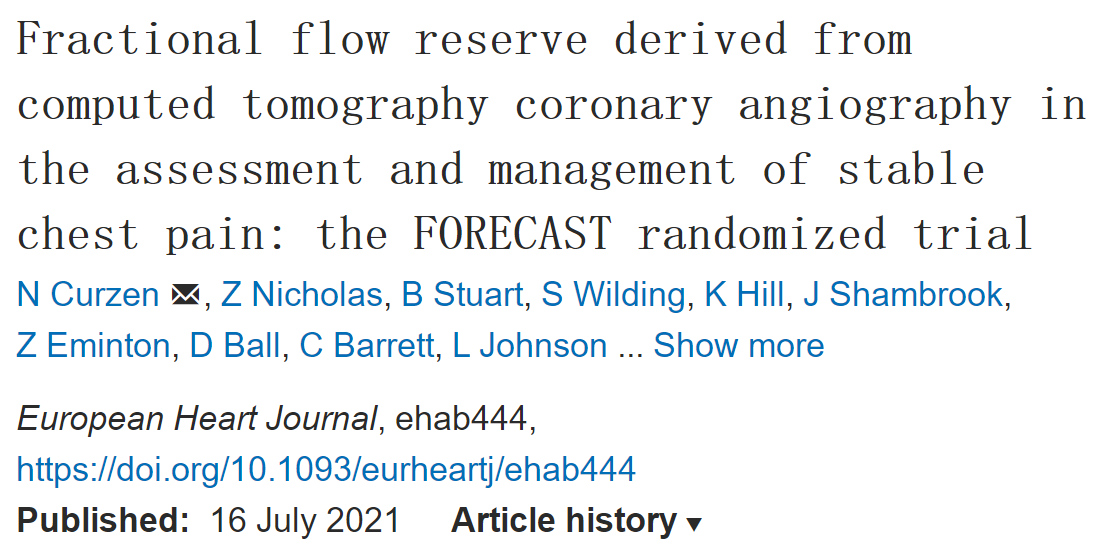
N Curzen.et al.Fractional flow reserve derived from computed tomography coronary angiography in the assessment and management of stable chest pain: the FORECAST randomized trial.European Heart Journal.2021.https://doi.org/10.1093/eurheartj/ehab444
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#稳定型#
62
#计算机#
60
#ART#
48
#冠状动脉造影#
70
#造影#
59
#HEART#
46