核酸治疗: miR-23b-3p是一个有希望的阿尔茨海默病治疗靶点
2022-05-31 生物谷 生物谷
研究者在体外和体内的研究结果提供了证据,表明miR-23b-3p通过减少tau过度磷酸化导致的细胞凋亡而在AD中发挥保护作用。
阿尔茨海默病(AD)是最常见的神经退行性疾病,以老年人记忆力减退、认知障碍和人格改变为主要临床特征。AD患者大脑的主要病理特征是存在由淀粉样蛋白b(Ab)组成的细胞外淀粉样斑块和由过度磷酸化的tau蛋白组成的细胞内神经原纤维缠结(NFTs),最终导致神经元丢失。
尽管有许多证据表明tau蛋白是抗体引发的神经变性的下游靶点,但尸检研究表明,AD症状的严重程度更多地与tau相关的病理程度有关,而不是抗体沉积。
在阿尔茨海默病(AD)中,脑内微小RNA(MiRNA)的异常表达可导致认知功能障碍和tau蛋白异常过度磷酸化。一些研究已经报道了microRNA-23b-3p(miR-23b-3p)在各种神经疾病中的作用;然而,它参与认知相关功能仍不清楚。
图片来源: https://doi.org/10.1016/j.omtn.2022.04.008.
近日,来自中国医学科学院和北京协和医学院的研究者们在Molecular Therapy: Nucleic Acids杂志上发表了题为“miR-23b-3p rescues cognition in Alzheimer’s disease by reducing tau phosphorylation and apoptosis via GSK-3b signaling pathways”的文章,该研究的发现有力地支持了miR-23b-3p在AD中发挥神经保护作用的假设,从而确定miR23b-3p是一个有希望的AD治疗靶点。
在本研究中,研究者探讨了miR23b-3p对AD的潜在治疗作用及其机制。淀粉样前体蛋白(APP)/早老素1(PS1)双转基因小鼠(APP/PS1小鼠)大脑皮质miR-23b-3p表达降低。这种减少在APPswe细胞、SAMP8小鼠脑和AD患者的血浆中得到证实。此外,与tau病理有关的主要tau蛋白激酶-3b(GSK-3b)被确定为miR-23b-3p的靶标。
体内功能研究表明,在APP/PS1小鼠脑室注射miR-23b-3p可通过抑制GSK-3b的表达和激活来改善认知障碍、组织病理学改变和多个部位的tau磷酸化免疫反应。同样,在APPswe细胞中miR-23b-3p的上调抑制了GSK-3b介导的tau过度磷酸化、AB1-42的产生和神经元的凋亡,导致GSK-3b/p-tau和Bax/caspase-3通路的抑制。
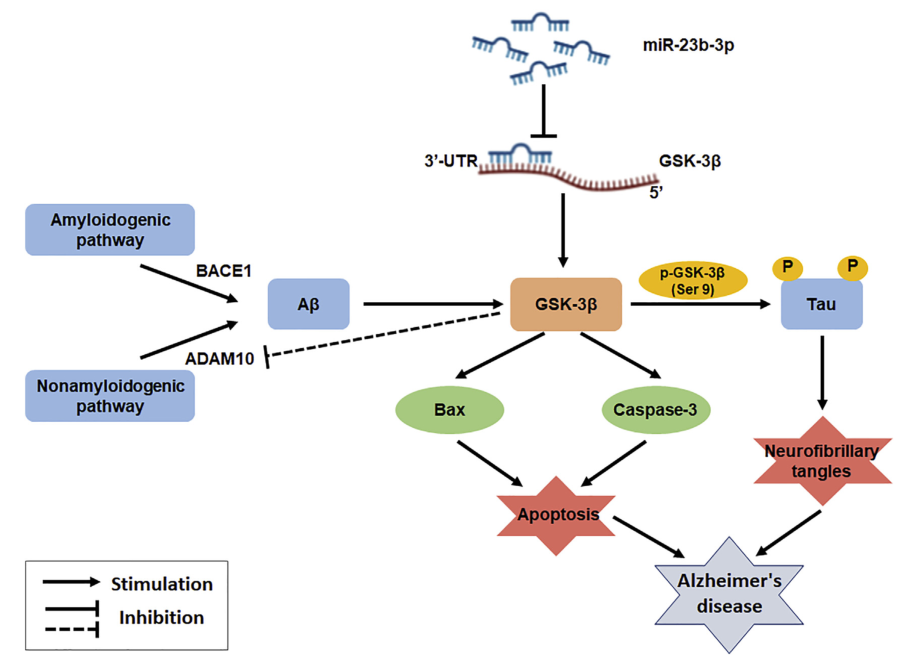
MiR-23b-3p通过抑制GSK-3b信号通路抑制AD细胞凋亡和tau磷酸化的可能机制
图片来源: https://doi.org/10.1016/j.omtn.2022.04.008
总之,研究者在体外和体内的研究结果提供了证据,表明miR-23b-3p通过减少tau过度磷酸化导致的细胞凋亡而在AD中发挥保护作用。MiR-23b-3p相关的神经保护机制可能是miR-23b-3p抑制脑内的GSK-3b。因此,miR-23b-3p是治疗AD的新的治疗策略的潜在靶点。
参考文献
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#阿尔茨海#
50
#阿尔茨#
58
#治疗靶点#
60
#miR#
67
#阿尔茨海默#
68