Nat Med:扼住命运的咽喉!斑马鱼帮助挽救重症淋巴病男孩
2019-07-06 苏煜静 生物探索
在丹尼尔10岁时,他有望成为一名足球运动员,那时他能够在25分钟里跑出5公里的距离。两年后,他的腿突然开始肿胀,出现呼吸困难的症状。医院诊断丹尼尔心脏周围有淋巴积液,并且淋巴液还在继续渗漏。
在丹尼尔10岁时,他有望成为一名足球运动员,那时他能够在25分钟里跑出5公里的距离。两年后,他的腿突然开始肿胀,出现呼吸困难的症状。医院诊断丹尼尔心脏周围有淋巴积液,并且淋巴液还在继续渗漏。
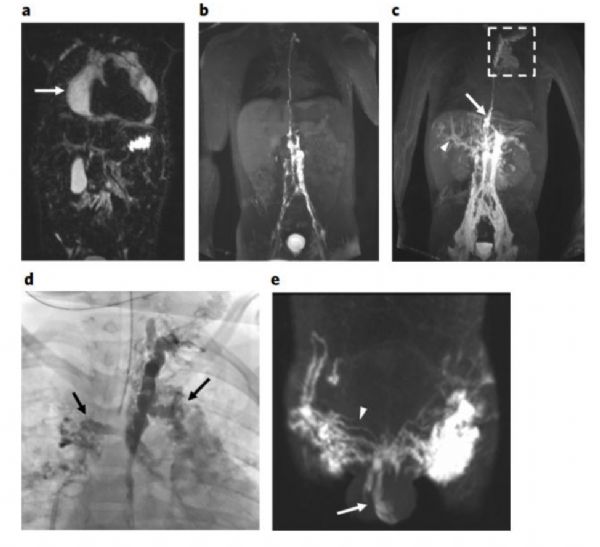
丹尼尔的胸部临床影像
丹尼尔的双腿和腹部像海绵一样肿胀。他的肺部充满了积液以至于只能靠着氧气罐勉强维持生命。在接受了一种西罗莫司(雷帕霉素)的免疫抑制药物治疗后,丹尼尔的情况并没有好转。费城儿童医院(CHOP)儿科肺科专家和应用基因组学中心主任Hakon Hakonarson博士说:“他的情况来越糟糕,死神正在向他招手。”
为了拯救这个脆弱的小生命,医护人员利用现有药物,重塑自身异常淋巴系统。这是一个危及生命的罕见疾病实施精准药物治疗的戏剧性案例。该研究发表在《Nature Medicine》杂志上。
斑马鱼帮忙找到病因
Hakonarson博士和同事认为找到疾病的基因根源才是丹尼尔唯一的希望。中枢导管淋巴异常可能是由几种基因突变引起的。因此,他们对丹尼尔进行了全外显子测序。
基因测序结果显示,十几个与淋巴异常相关的基因看起来都很正常。但是他的X染色体上缺少了一个叫做ARAF的基因。这种基因会产生一种叫做激酶的酶,这种酶能够将分子添加到细胞的蛋白质中。这种物质太多会导致细胞过度增殖,以至于发生癌变。
然而,人们从未发现ARAF突变与淋巴疾病相关。为了确定这个基因的缺失是否是丹尼尔患病的罪魁祸首。科学家们对斑马鱼进行了基因改造,使其携带这种突变。
研究人员通过将ARAF突变基因插入斑马鱼的胚胎中来探索其功能。五天内,斑马鱼便形成了类似的异常淋巴管。这证明了ARAF突变导致淋巴管过度生长。
Christoph Seiler说:“随着ARAF基因的突变,这条四分之一英寸长的鱼长出了淋巴管,淋巴管不断地生长,就像丹尼尔的淋巴管一样。”
老药新用,黑色素瘤药物转变战场
治疗ARAF突变的药物有十种。研究人员将药物放入水中发现,斑马鱼在吸收药物后淋巴管停止扩散,并且没有对其他部分造成伤害。
这些药物都是MEK抑制剂,通常用于黑色素瘤患者。尽管医生可以为FDA批准的病症开出药物,但Hakonarson不愿这么做。他说:“我们不想冒险给孩子服用一种有毒的成人药物,除非专家认为潜在的好处大于风险。”
最终,CHOP肿瘤学团队的Jean Belasco博士在获得FDA的同意许可后给丹尼尔使用了名为trametinib的MEK抑制剂。
在开始实验治疗后的两个月内,丹尼尔的呼吸得到改善。开始治疗三个月后,他肺部的积液开始减少,并且脱离呼吸机开始进行自主呼吸新鲜空气。MRI显示他的淋巴管正在重塑。丹尼尔双腿的肿胀也在逐渐消失。
结语
这项研究首次证明了一种药物可以完全重塑整个器官系统,并为许多患有类似淋巴管流动障碍的患者带来了希望。
现年14岁的丹尼尔已经恢复大部分正常活动,例如骑自行车、打篮球以及其他训练,如举重和指导足球训练等。他的母亲说:“就在两年多前,丹尼尔必须在家里依靠轮椅接受辅导。现在他回到学校和朋友们一起活动。”
原始出处:
Dong Li, Michael E. March, et al. ARAF recurrent mutation causes central conducting lymphatic anomaly treatable with a MEK inhibitor. Nature Medicine. Jul 2019.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#Nat#
63
#斑马鱼#
97
#Med#
68
神奇
103