哮喘新药:再生元的Dupixent能够迅速改善儿童的肺功能
2021-05-19 Allan MedSci原创
VOYAGE试验评估了Dupixent联合标准护理(SoC)在408例中度至重度哮喘不受控制的患儿中的安全性和有效性。
哮喘是常见的气道慢性炎症疾病,主要特征是多变和复发的症状、可逆性气流阻塞,和支气管痉挛。常见症状表现为喘息、咳嗽、胸腔紧迫、胸闷和呼吸困难。普遍认为哮喘是因为基因和环境因素共同导致的。环境因素通常包含:暴露于空气污染和过敏原,其他可能的诱发因子包含阿司匹林和β受体阻断药之类的药物。
根据一项III期试验的详细结果,赛诺菲和Regeneron的Dupixent可显著降低6至11岁患有中度至重度哮喘不受控制的儿童的严重哮喘发作,并迅速改善其肺功能。
此外,在VOYAGE试验中,发现Dupixent(dupilumab)可改善总体哮喘控制并减少呼出气一氧化氮(FeNO)的含量,FeNO是2型炎症的气道生物标志物,在哮喘中起关键作用。

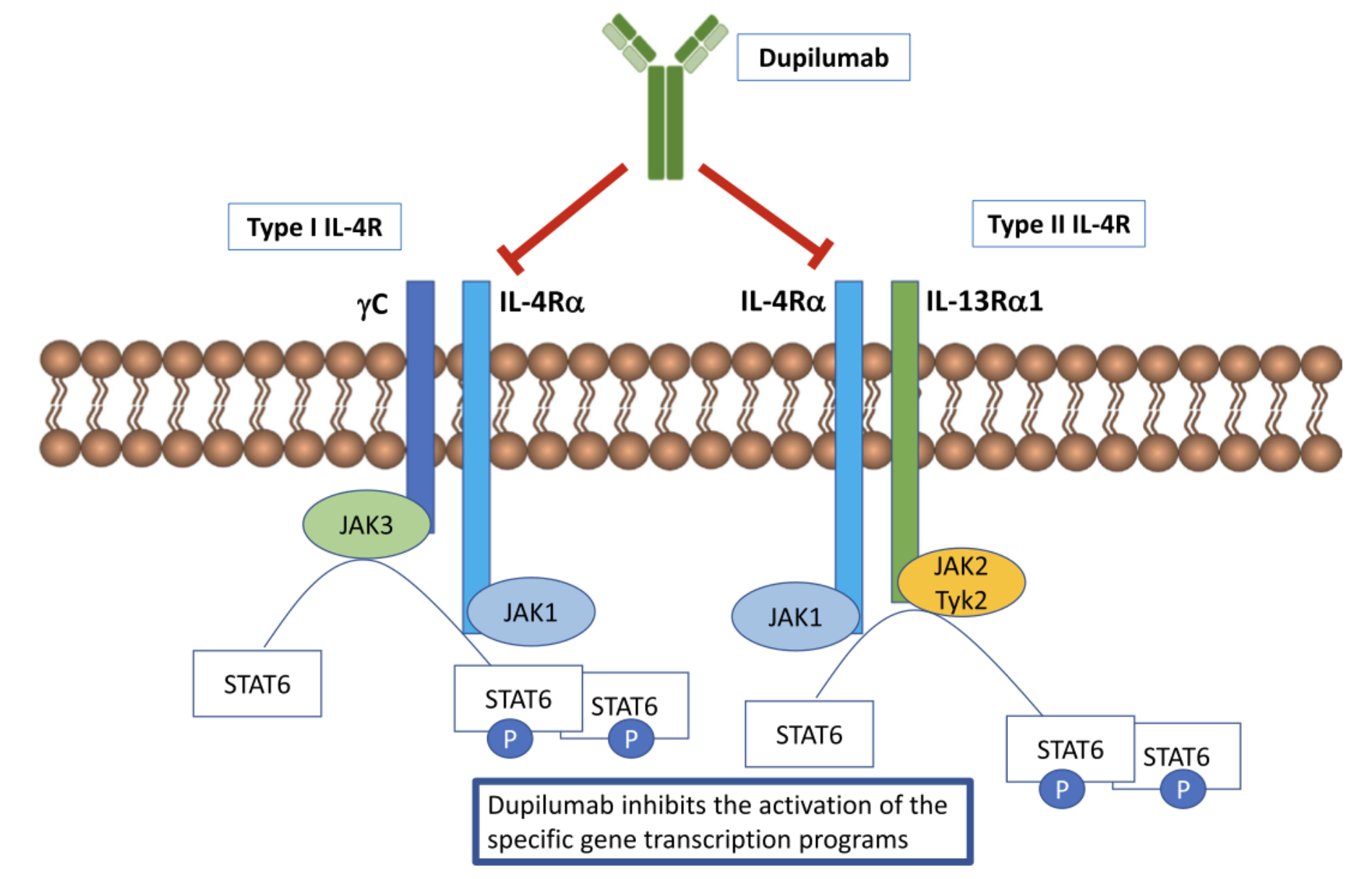
图1. Dupixent(dupilumab)的作用机制
该试验的主要研究者Leonard Bacharier说:“患有不受控制的中度至重度哮喘的儿童会经历严重且持续的症状,这些症状可能影响他们生活的许多方面,包括学习、睡眠和运动”。
他补充说:“试验结果表明,将dupilumab加入标准的护理治疗后,可显著减少哮喘发作,迅速改善肺功能并改善哮喘控制,这对于这些患儿是尤其重要的”。
VOYAGE试验评估了Dupixent联合标准护理(SoC)在408例中度至重度哮喘不受控制的患儿中的安全性和有效性。这项研究的主要结果(先前于2020年10月报道)发现,与安慰剂相比,Dupixent联合SoC治疗组患者的严重哮喘发作率显著降低(一年平均降低65% vs. 59%)。病人的肺功能也有所改善,最早可在两周内观察到并持续长达52周。
原始出处:
http://www.pharmatimes.com/news/sanofis_dupixent_rapidly_improves_lung_function_in_children_1370186
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#Dupixen#
84
受益匪浅
85
结果令人鼓舞
95
#Dupixent#
66
学习了
90
很好
117