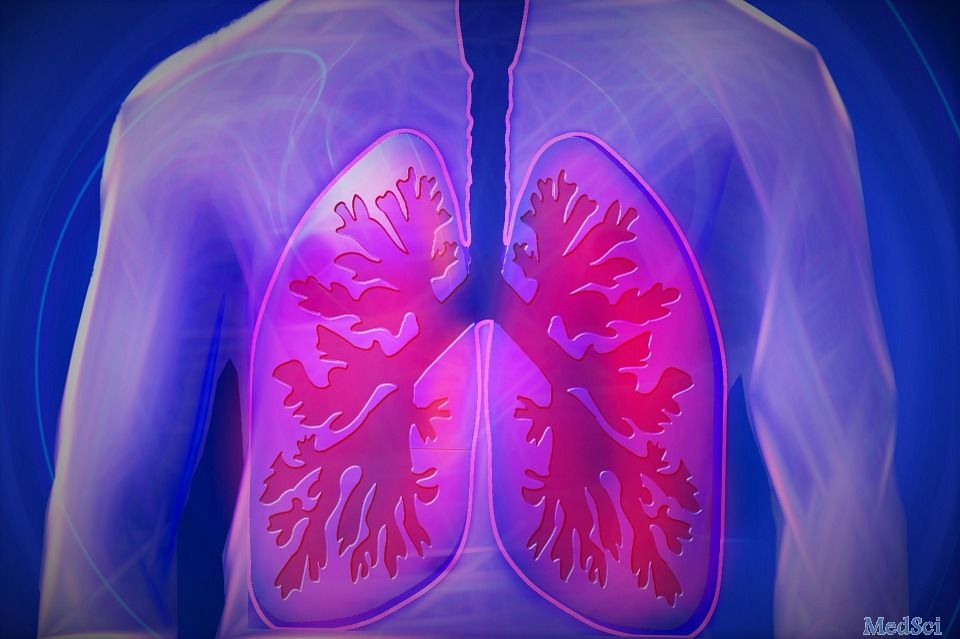
Nature Commun:TGF-β信号通路激活导致肺动脉高压的原因
2017-06-01 MedSci MedSci原创
血小板反应蛋白-1(thrombospondin-1, TSP-1)能够引起TGF-β信号通路的激活,而这一激活对于足够使血吸虫感染的小鼠发展肺动脉高压,并且是必需的。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#动脉高压#
61
#Nat#
59
#COMMUN#
78
#TGF#
73
学习
98
学习了,不错?
101
#信号通路#
68
#TGF-β#
71
学习了,谢谢分享
98
靶向TSP-1抑制依赖其激活的TGF-β的信号激活可能是未来治疗肺动脉高压的潜在方法。
100