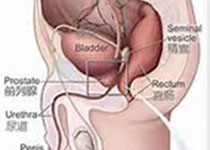
Sci Rep:转移前列腺癌中HOXB13同源异型盒基因能够调控有丝分裂蛋白激酶互作网络
2019-07-21 AlexYang MedSci原创
HOXB13是一个同源异型盒转录因子,并且与根治性前列腺切除术后复发有关。虽然HOXB13能够以环境依赖的方式来调控雄激素受体(AR)功能,它在前列腺癌(PC)转移中的关键影响仍旧大部分未知。最近,有研究人员为了鉴定转移性PCs中HOXB13的转录靶标,在人类前列腺肿瘤特异性AR结合位点附近进行了综合的差异化基因表达(DEGs)生物信息学分析。无监督主成分分析(PCA)表明HOXB13靶基因聚焦于
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#蛋白激酶#
88
#互作#
85
#激酶#
67
#有丝分裂#
95
前列腺癌相关研究,学习了,谢谢梅斯
81