Front Oncol:化疗对转移性前列腺癌患者的总生存期影响
2021-11-29 yd2015 MedSci原创
该真实世界数据研究表明,化疗可以改善转移性前列腺癌患者的总生存期。但是,总生存获益的幅度无法与III期试验相媲美。
随机临床试验(RCT)证实化疗改善了转移性前列腺癌患者的总生存期。然而,真实世界中仍缺乏大规模流行病学数据验证这一疗效。所以,真实世界中化疗是否能够改善转移性前列腺癌患者预后尚不能肯定。因此,国外学者开展了相关研究,评估化疗对于转移性前列腺癌患者的总生存期的影响。相关结果发表在Frontiers in Oncology杂志上。
该研究通过筛查2014年-2015年SEER数据库中确诊的新转移性前列腺癌患者。Kaplan-Meier和Cox回归模型分析化疗暴露患者与无化疗患者之间的总生存差异。所有分析在倾向-评分匹配(PSM)的队列中重复。
在2014年至2015年期间,筛查了4295例新转移性前列腺癌患者。其中905例(21.1%)患者接受了化疗。与无接受化疗的患者相比较,接受化疗的患者更年轻(64岁vs 70岁P<0.001)、PSA >90 ng/ml患者比例更高(57.3 vs 51.8%, p=0.01)、GGG V患者比例更高(52.3 vs 43.6%, p=0.01)、cN-1期患者比例更高(44.5 vs 31.6%,p<0.001)和cM1c期患者比例更高(19.8 vs 14.6%,p<0.001)。局部治疗类型无显著差异。

临床特征
PSM前,基于整体队列,包括905例接受化疗和3390例无化疗患者。化疗和无化疗患者的18个月和30个月的总生存率分别为76.3 vs 69.3%和61.6 vs 54.3%。在多变量Cox回归模型中,与无化疗患者相比,化疗患者表现出更低的总死亡风险(HR:0.82, CI: 0.72- 0.96, p=0.01)。

PSM前OS对比
经过PSM后,该队列包括879例接受化疗和1611例无化疗患者。各临床病理特征均平衡。化疗患者和无化疗患者的18个月和30个月的总生存率分别为76.3 vs 70.5%和61.6 vs 56.0%。同样在多变量Cox回归模型中,与无化疗患者相比,化疗患者表现出更低的总死亡风险(HR:0.77, CI: 0.66-0.90,p<0.001)。
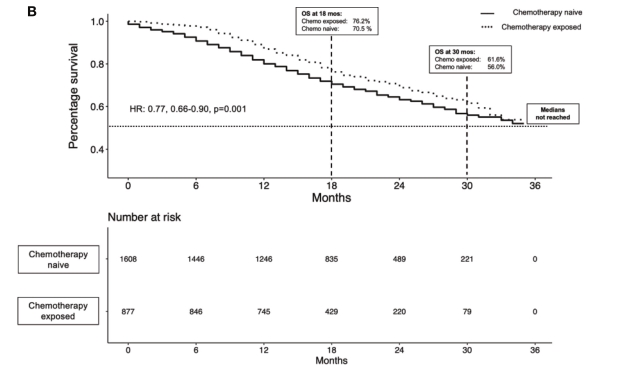
PSM后OS对比

多因素分析相关因素
综上,该真实世界数据研究表明,化疗可以改善转移性前列腺癌患者的总生存期。但是,总生存获益的幅度无法与III期试验相媲美。
原始出处:
Hoeh B, Würnschimmel C, Flammia RS, Horlemann B, Sorce G, Chierigo F, Tian Z, Saad F, Graefen M, Gallucci M, Briganti A, Terrone C, Shariat SF, Tilki D, Kluth LA, Mandel P, Chun FKH and Karakiewicz PI (2021) Effect of Chemotherapy on Overall Survival in Contemporary MetastaticProstate Cancer Patients. Front. Oncol. 11:778858. doi: 10.3389/fonc.2021.778858
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncol#
87
#转移性前列腺癌患者#
73
#生存期#
68
#转移性#
61
#转移性前列腺癌#
85
#总生存期#
69