The Lancet Oncology:前列腺癌患者术后生活质量调查
2017-04-01 MedSci MedSci原创
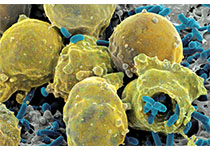
如何选择早期前列腺癌的治疗方案极大影响患者的预后生活质量
对相应人群的前瞻性研究表明,根治性前列腺切除术、放疗等疗法的治疗副作用对于新诊断的局限性前列腺癌患者的预后生活质量有很大影响。
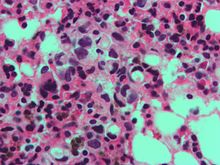
研究人员在治疗后的第3、12、24个月,通过电话对患者进行随访,对术后症状进行评分(0-100,分数越高,功能丧失症状越严重)。1141名患者中,有469名(41%)接受前列腺切除术、109人(10%)接受浅部放射治疗、249人(22%)接受体外放射治疗、314名(28%)接受主动的病情监测(保守治疗)。
在治疗3个月后,性功能障碍最严重的群组为前列腺切除术组,分数为36.2分、体外放射治疗组为13.9分、浅部放射治疗组为17.1分;前列腺切除术组尿失禁最严重为33.6分;尿路梗阻疼痛现象最严重的为浅部放射治疗组,20.5分;肠道症状最严重的为体外放射治疗组,4.9分。在第24个月主要不良症状的得分没有显着改变。
研究表明,相比于其他的治疗手段,根治性前列腺切除术更容易导致尿漏与性功能障碍;采用放射治疗的病人2年后的生活质量与保守治疗相近,这项研究将帮助医生和患者做出一个既不影响治疗也不降低患者预后生活质量的决定。
原文出处:
Priya Venkatesan et al. Quality of life after treatments for prostate cancer. The Lancet Oncology. 2017 Mar 30.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncology#
60
#Oncol#
56
#Lancet#
67
要好好学习研究下
81