本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

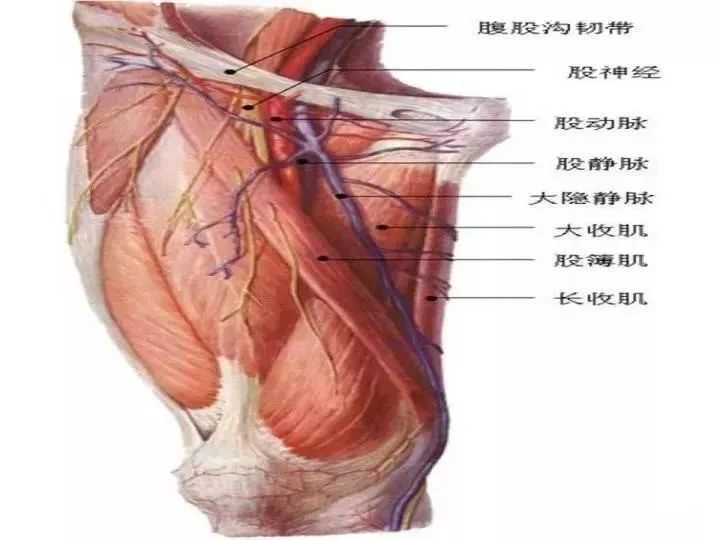
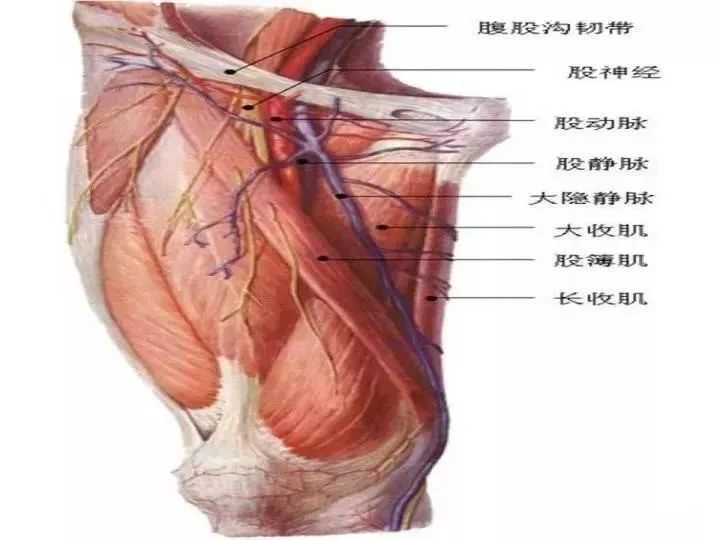

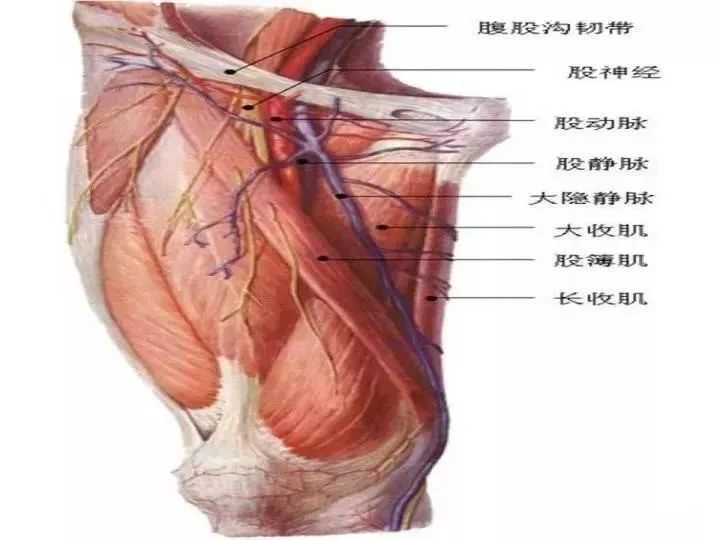
PCI主要并发症包括:①急性性冠脉闭塞;②无复流;③冠脉穿孔;④支架血栓形成;⑤支架脱载;⑥出血;⑦血管并发症:股动脉穿刺主要并发症如穿刺点及腹膜后血肿、假性动脉瘤、动静脉瘘、动脉夹层和(或)闭塞;桡动脉穿刺主要并发症如桡动脉术后闭塞、桡动脉痉挛、前臂血肿、筋膜间隙综合征、假性动脉瘤;⑧对比剂导致的急性肾损伤等。
对于接受经皮冠脉介入治疗的急性冠脉综合征患者来说,术后氯吡格雷治疗期间如果出现血小板高反应性,意味着发生缺血事件的风险较高。
在近日召开的EuroPCR会议上,GLOBAL LEADERS研究的最新事后分析结果表明,对于复杂冠脉介入治疗(PCI)术后患者,与标准抗血小板治疗策略(1年双联抗血小板治疗+1年阿司匹林)相比,长期单用替格瑞洛策略(1个月双联抗血小板治疗后单用替格瑞洛)可能更好。
1月30日,阜外医院李建军教授研究团队联合北京宣武医院、北京安贞医院研究人员发表的一项多中心、前瞻性队列研究提示,在冠脉介入术后的稳定性冠心病患者中,血浆脂蛋白(a)[Lp(a)]水平对心血管事件有较好的预测价值,Lp(a)水平高(≥30 mg/dl)者预后不良。研究者认为,在行择期经皮冠脉介入术前进行血浆Lp(a)水平,对于稳定性冠心病患者的风险分层、临床治疗决策制定(降脂治疗强度、传统的可控危
近年来,冠脉介入治疗技术得到了快速发展,很多医院都展开了这项技术,它在诊疗心血管疾病方面具有诸多优势,已经成为治疗急性冠状动脉粥样硬化性疾病的首选方案,极大降低了冠心病的致残率和死亡率,但是该项技术是一种有创伤性的治疗措施,术后出现一些并发症是不可避免的,下面介绍一下常见的5种致命性冠脉介入并发症,供大家参考。一、术后支架内血栓形成支架内血栓形成是一个灾难性的并发症。中国多中心药物洗脱支架急性
近期,阜外医院杨跃进、俞梦越等代表表北京市心血管介入质量控制与改进中心专家委员会,对2009年1月至2018年12月北京市56家医院共473 411 例冠心病患者死亡率进行了分析。


梅斯医学MedSci APP
医路相伴,成就大医
#并发#
78
棒 学习了
65
学习了
63
#冠脉介入术#
92
要点总结,实用!
91
学习了
77