ARVO 2016:角膜内皮营养不良及抗角膜新生血管治疗的前沿热点
2016-06-19 佚名 国际眼科时讯
2016的视觉与眼科学会协会(ARVO)年会上,作为第一作者,Keisuke Ogata和Crystal Shin阐述了他们的在角膜疾病领域的新发现。Keisuke OgataFuchs角膜内皮营养不良(FECD)是最常见的基因遗传性角膜营养不良。虽然对其基因背景所知甚少,梅约诊所的Wieben等人报道了在FECD患者中常可观察到转录因子4(TCF4)中三核苷酸重复扩增。Keisuke Ogata
2016的视觉与眼科学会协会(ARVO)年会上,作为第一作者,Keisuke Ogata和Crystal Shin阐述了他们的在角膜疾病领域的新发现。
Keisuke Ogata
Fuchs角膜内皮营养不良(FECD)是最常见的基因遗传性角膜营养不良。虽然对其基因背景所知甚少,梅约诊所的Wieben等人报道了在FECD患者中常可观察到转录因子4(TCF4)中三核苷酸重复扩增。Keisuke Ogata团队以及其他团队随后的研究结果已证实了这个惊人的发现。
在这个研究中,Keisuke Ogata团队对大量的FECD患者进行了基因组DNA检测。当前的结果进一步证实了TCF4中三核苷酸重复扩增为FECD的共同基因背景。未来,如三核苷酸重复扩展如何导致疾病以及对没有三核苷酸重复扩展的患者的基因背景的阐释的相关话题将会为FECD的诊断和治疗提供新的研究方向。
Crystal Shin
为保持清晰的视觉,正常健康的眼最外的透明层(角膜)是没有任何的血管的。眼表面的任何损伤都会刺激血管长入角膜,称之为角膜新生血管(CNV),如果不予治疗可导致严重的视力丧失甚至失明。虽然滴眼液治疗非常简便,但是有效性不足,必须每天多次使用,可能造成毒性副作用。
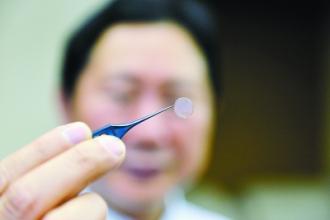
关于如何快速有效治疗CNV,Crystal Shin教授的团队发明了一种新的使用糖聚合物硫酸葡聚糖(DS)的纳米镜片(Nanowafer)。Nanowafer为一层透明薄膜,如角膜接触镜样简单覆盖在眼表。Nanowafer在药物释放时溶解并消失。
Crystal Shin教授的团队研究了Nanowafer对小鼠眼化学伤的有效性。研究表明了Nanowafer治疗在防止CNV和角膜混浊形成上的有效性为滴眼药物的两倍。Nanowafer的出现是眼部疾病如干眼、青光眼、眼部感染和外伤等有效治疗的一项主要进展。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ARVO#
40
#新生血管#
33
赞一个!好文章拜读了,认真学习了。
65
继续学习
55
继续关注
69
深度好文,赞一个!!!
69
非常不错,值得学习
72
#角膜#
26
这个不错
62
值得查看
81