72个抗肿瘤靶向药物全景报告!
2016-07-21 Armstrong 生物制药小编
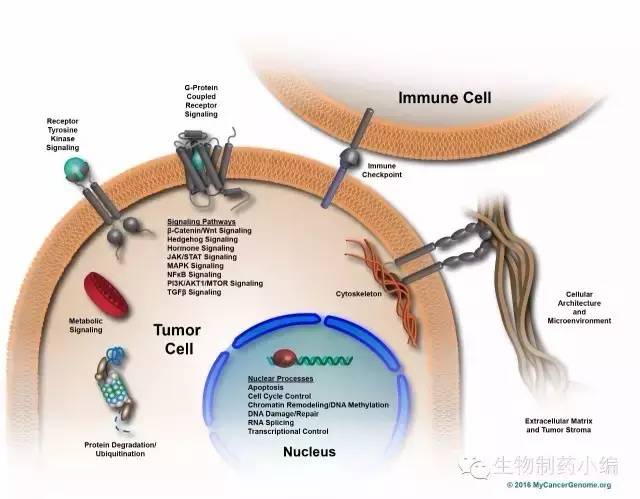
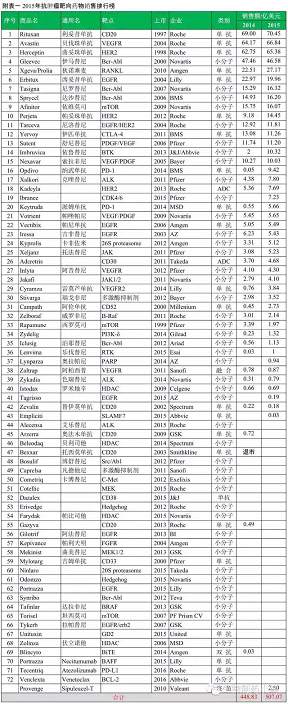
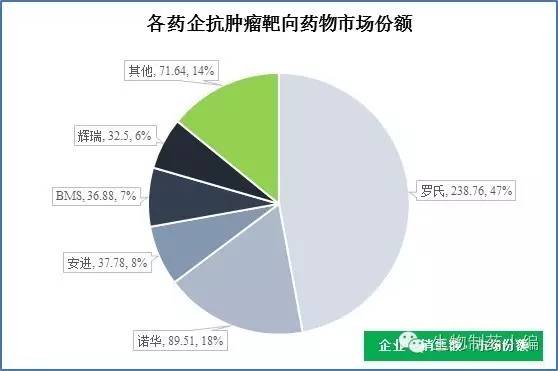
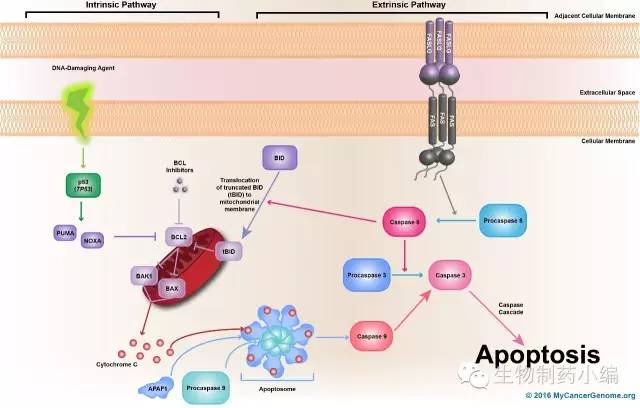
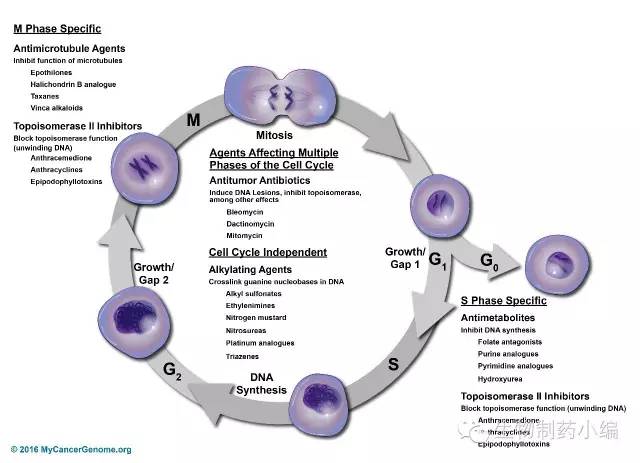
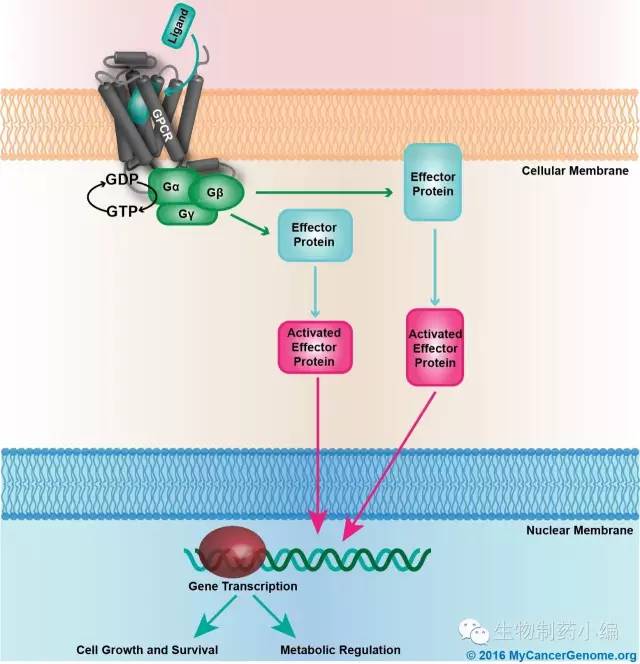
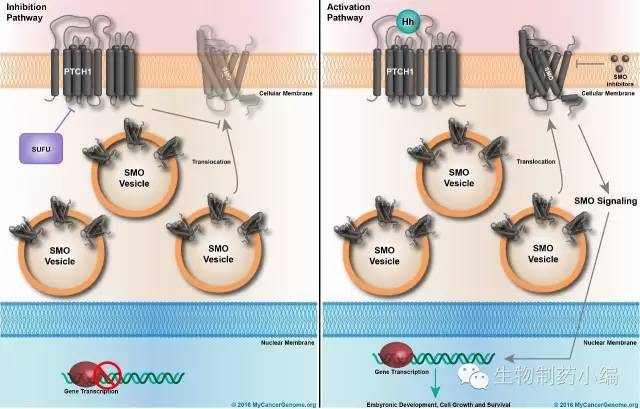
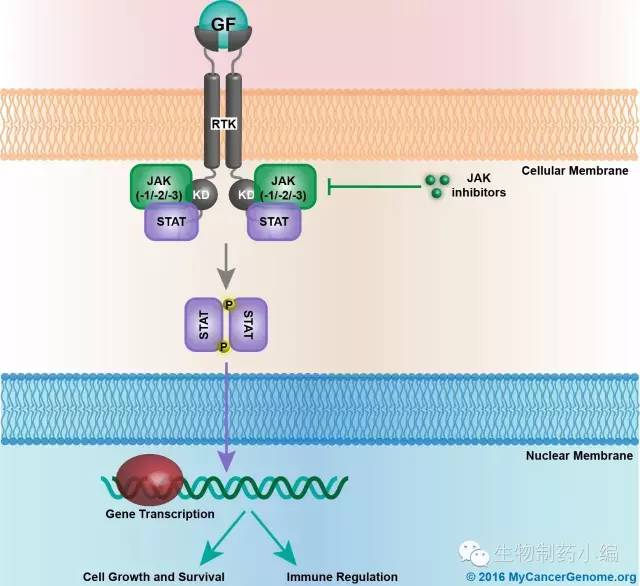
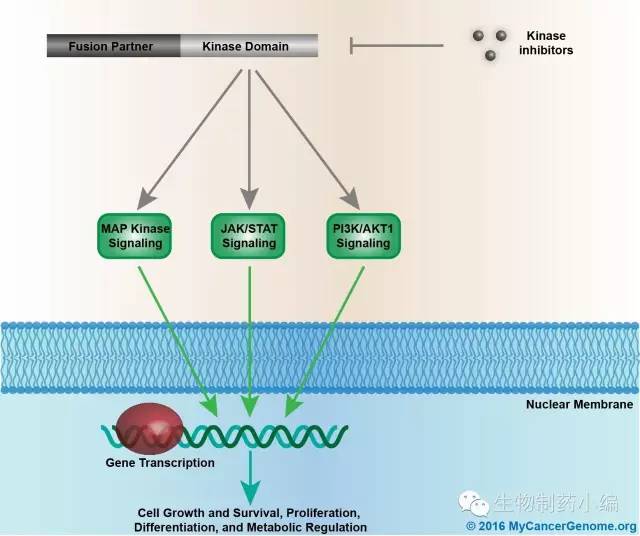
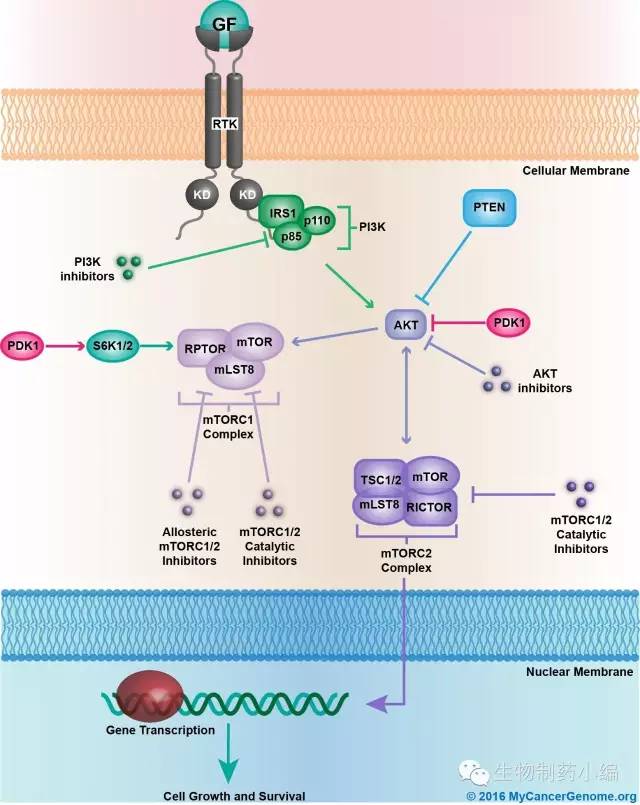
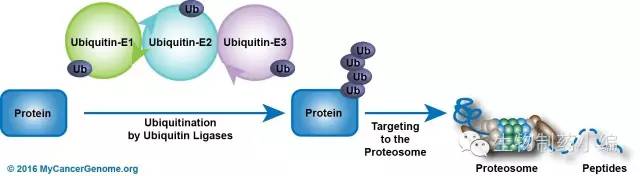
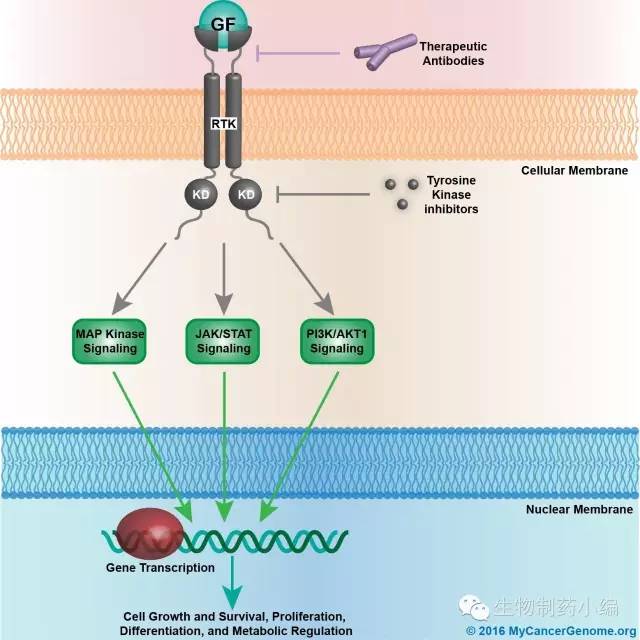
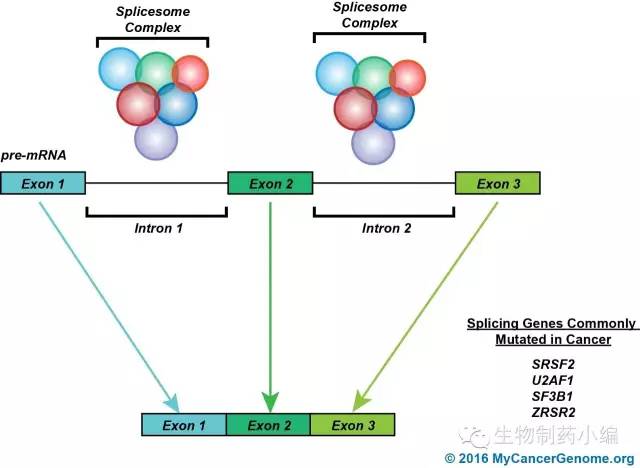
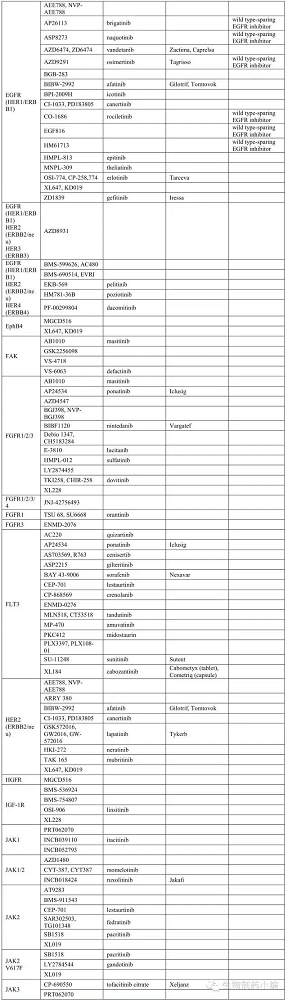
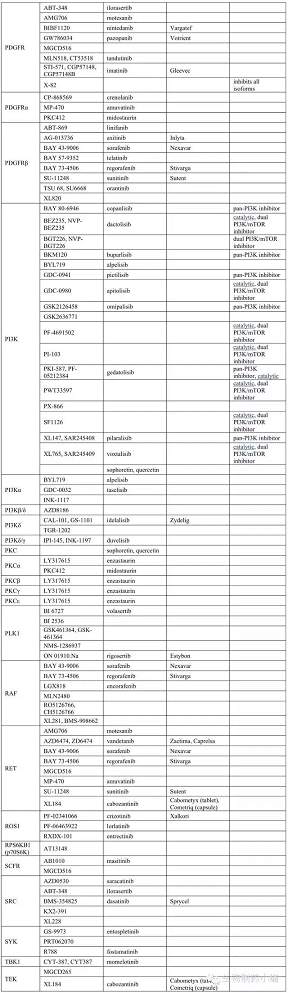
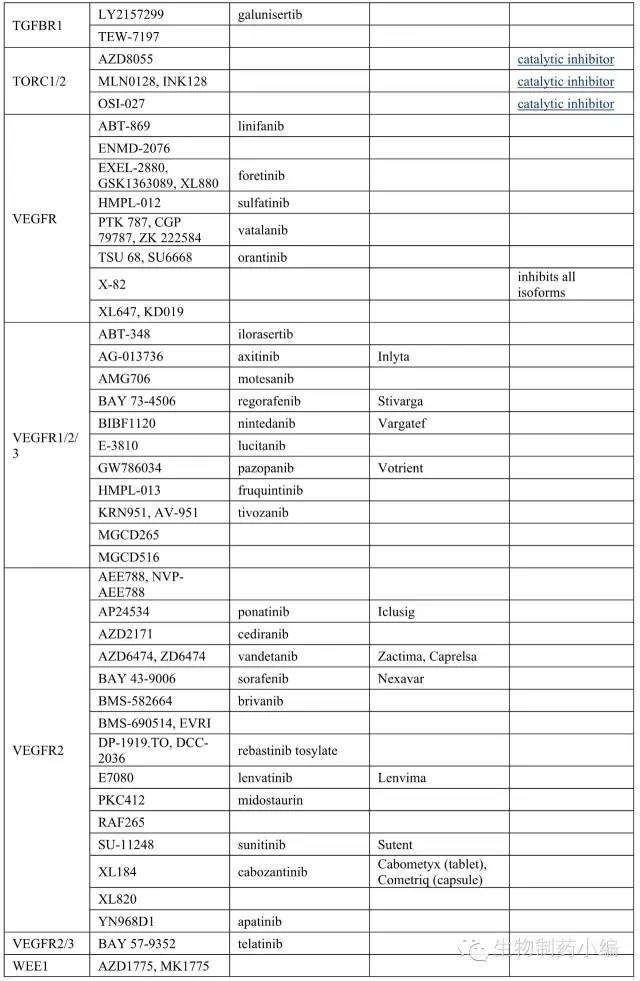
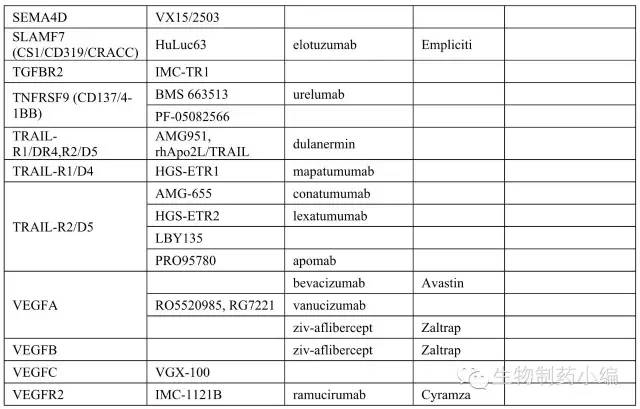
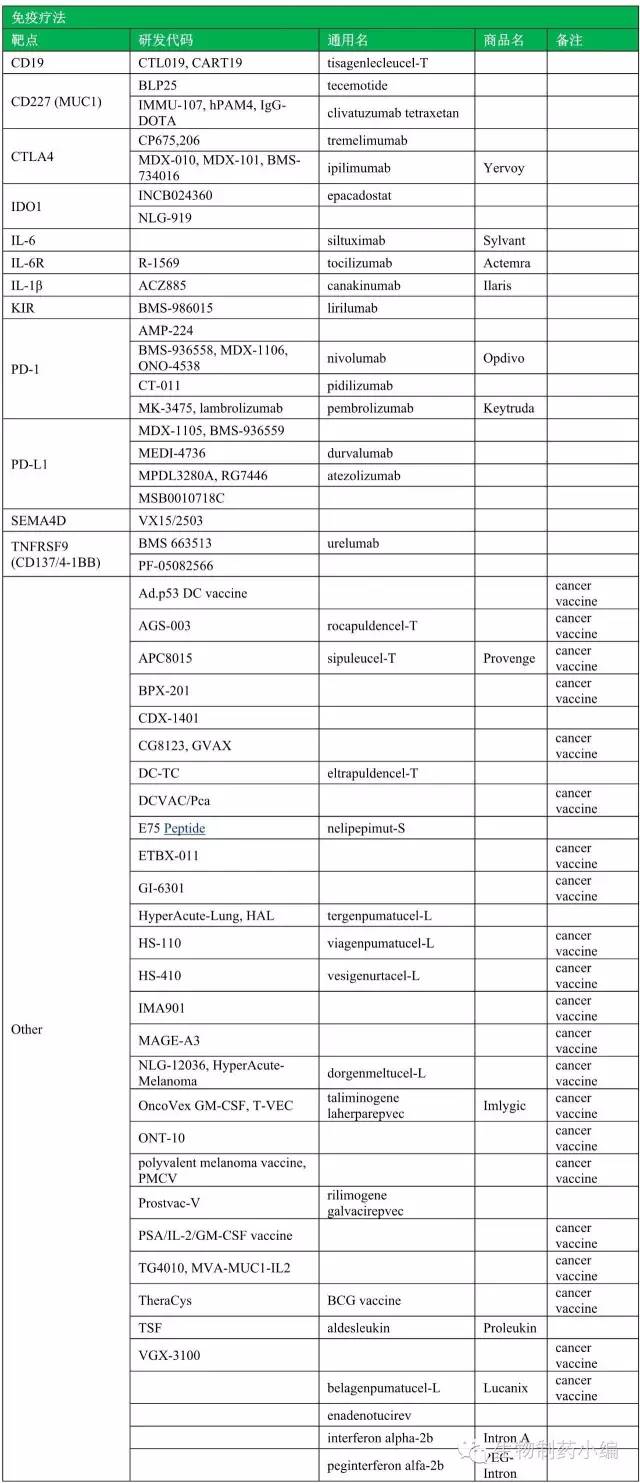
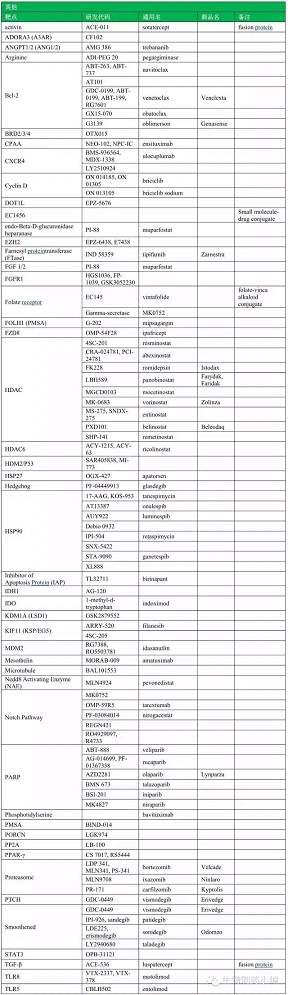
2016年初,Nature曾专文介绍FDA批准的45款抗肿瘤靶向药物,主要介绍激酶抑制剂和抗体药物。本文将从更广泛的范围梳理抗肿瘤靶向药物,包括更完整的靶向抗肿瘤药物范围,补充市场格局、信号通路介绍等方面信息,描绘一幅更完整的全景图。 靶向药物极大改变了肿瘤等适应症的治疗局面:副作用小、疗效显著,改善患者生存质量的同时,也创造了巨大的市场机会。 一、靶向药物统计















本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#肿瘤靶向#
74
#全景#
68
不错 值得收藏
93
赞了!深度好文,深入学习。
89
学习了,有意思
90
继续努力
102