本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

2017-07-13 sunshine2015 环球医学
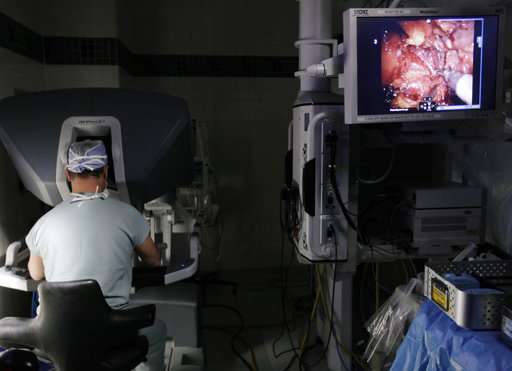
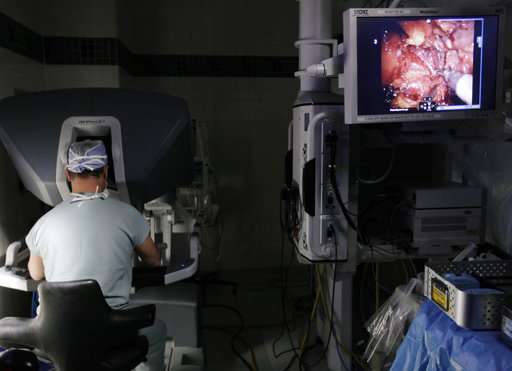
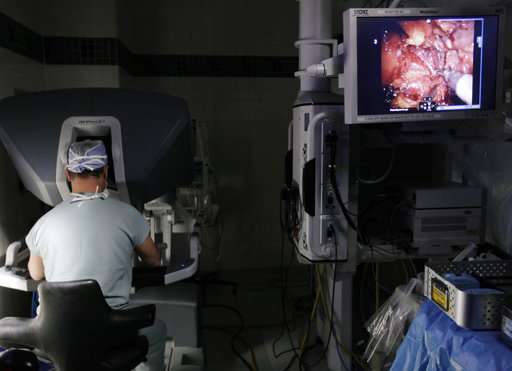
活检显示癌症,所以你必须快速行动,对吧?不一定,如果是前列腺肿瘤。

导管上皮非典型增生(ADH)是乳腺癌的危险因素。研究者进行了一项研究,比较不同诊断方式(空芯针穿刺活检 vs 切除活检)下的ADH与浸润性乳腺癌风险之间的联系。 队列研究比较了955 331名进行钼靶筛查女性的浸润性乳腺癌10年累积风险(诊断或未诊断ADH)。数据来自于5个乳腺影像学注册数据库。其中1727例ADH患者,空芯针穿刺活检和切除活检分别诊断了1058 (61.3%)例和635 (
约有三分之二的成年人都有甲状腺结节,不过大部分都属于良性结节或发展缓慢的肿瘤,不会对生命造成威胁。据统计,约有四分之三的女性甲状腺癌患者和近一半的男性甲状腺癌患者的肿瘤不会导致任何症状或死亡,即便他们不做活检或切除手术。
为了帮助大家更好的分离囊泡、提取RNA、存储样本和分析数据,The Scientist杂志与多位专家学者探讨了检测不同血液生物学指标的策略,贡献出了相应的注意事项和实验技巧。
因此,CD68+白细胞浸润的数字高分辨率评估显著提高了早期肾脏移植活检的预后价值。
随着内镜技术的普及与发展,胃黏膜活检已成为病理诊断中最常见的项目之一。为了使病理诊断达到更好的一致性,能够准确、科学地为治疗提供参考,中华医学会病理学分会消化病理学组制定了本共识。本共识的出台,可进一步提高胃黏膜活检标本病理诊断的准确性,为临床进一步诊疗提供可靠、合理的病理依据。
随机活检被推荐用于溃疡性结肠炎(UC)相关的结直肠癌的监测。然而,有针对性的活检可能是更有效的。我们进行了一项随机对照试验,对UC患者针对性的或随机活检的瘤样检出率进行了比较。 研究纳入了246名UC病程≥7年的患者,来自日本的52个机构(2008年10月1日至2010年12月31日)。患者被随机分配到随机组(除了有针对性的活组织切片检查外,每10厘米收集活检标本, n=122)或针对目标组


梅斯医学MedSci APP
医路相伴,成就大医
#Engl#
60
#Eng#
65
#Med#
55
学习一下谢谢分享
80
有道理
74
学习了学习了学习了学习了
81
学习了谢谢分享
0