日研究首次弄清了非酒精性脂肪肝的发病机制
2012-07-09 庄云芳 新华网
文献标题:Hyperresponsivity to Low-Dose Endotoxin during Progression to Nonalcoholic Steatohepatitis Is Regulated by Leptin-Mediated Signaling文献来源:Cell Metabolism 2012 july ;16(1):44-54 &nb
文献来源:Cell Metabolism 2012 july ;16(1):44-54

非酒精性脂肪肝多由肥胖引起。它是指患者无饮酒史,但病理学上和酒精性脂肪肝患者有相似的病理状态,比如也有肝细胞脂肪变性、肝小叶炎症,有时也有“酒精”玻璃样变性和肝纤维化等。
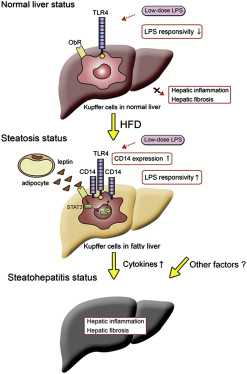
研究人员在动物实验中发现,实验鼠肥胖后,脂肪细胞大量分泌的肥胖基因编码产物Leptin会发挥作用,促使肝脏对肠内细菌分泌的毒素脂多糖发生过敏反应,从而导致肝部疾病。
横滨市立大学教授中岛淳说:“如同花粉症患者一样,肥胖者会对细菌发生过敏反应,这一发现将有助于开发新的诊疗方法。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了,如果附有这方面的文献链接就好了。
135
#酒精性脂肪肝#
77
#酒精性#
87
#非酒精性#
64