JAHA:循环中PCSK9水平与动脉硬化相关吗?
2017-05-07 xing.T MedSci原创
在布里西盖拉心脏研究中,循环PCSK9水平是动脉硬化显著相关,并且独立于性别以及女性的绝经状态。
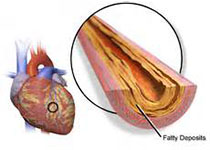
循环中人类枯草溶菌素转化酶9(PCSK9)的水平与心血管事件风险增加显著相关。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员旨在通过一个大样本的总体健康参与者来评估循环中PCSK9水平与动脉硬化之间的相关性,而动脉硬化是心血管疾病风险的早期生物标志。
该研究的参与者来自于布里西盖拉心脏研究的历史队列,研究人员将其中的主动吸烟者排除后,纳入了进行心血管疾病二级预防并且接受他汀类药物或血管扩张剂治疗的参与者,研究人员选择了227名绝经前妇女、193名年龄匹配的男性、460名绝经后妇女和416名年龄匹配的男性参与者。在这些参与者中,研究人员评估了血浆中PCSK9水平与脉搏波传导速度之间的相关性。
研究人员发现绝经后妇女血浆中PCSK9水平(309.9±84.1纳克/毫升)较高,相比于其他组参与者(P<0.001)。老年男性PCSK9水平显著高于青年男性(283.2±75.6 vs. 260.9±80.4毫微克/毫升;P=0.008)。在整个样本中,脉搏波速度主要通过年龄(B=0.116,95%可信区间为0.96-0.127,P<0.001)、PCSK9(B=0.014,95%可信区间为0.011-0.016,P<0.001)和血清尿酸(B=0.313,95%可信区间为0.024-0.391,P=0.026)来进行预测。体育活动、低密度脂蛋白胆固醇、高密度脂蛋白胆固醇和估算的肾小球滤过率与脉搏波速度无关(P>0.05)。考虑到亚组描述,年龄和PCSK9水平主要与脉搏波传导速度有关,在绝经后妇女中也与血清尿酸有关。
在布里西盖拉心脏研究中,循环PCSK9水平是动脉硬化显著相关,并且独立于性别以及女性的绝经状态。
原始出处:
Massimiliano Ruscica,et al. Circulating Levels of Proprotein Convertase Subtilisin/Kexin Type 9 and Arterial Stiffness in a Large Population Sample: Data From the Brisighella Heart Study.JAHA.2017. https://doi.org/10.1161/JAHA.117.005764
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Csk#
84
#PCS#
64
学习一下知识了
83
学习一下知识
95
谢谢了,学习
96
好文,值得点赞,更值得收藏!慢慢领会学习的。给点个赞!
93
#AHA#
62
很好的学习了
106
动脉硬化是早期心脏病的标志
50
学习过了,涨知识了!!!
69