Hepatology:2D-MRE诊断NAFLD进展期肝纤维化
2014-12-10 MedSci MedSci原创
Fig1. Diagnostic accuracy of MRE for advanced fibrosis. AUROC for the detection of advanced fibrosis in patients with biopsy-proven NAFLD is shown, and a two-tailed P value is provided. TPR, true po
Fig1. Diagnostic accuracy of MRE for advanced fibrosis. AUROC for the detection of advanced fibrosis in patients with biopsy-proven NAFLD is shown, and a two-tailed P value is provided. TPR, true positive rate; FPR, false-positive rate.
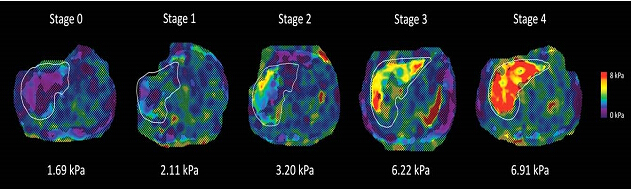
Fig3. MRE stiffness maps of 5 patients with NAFLD and different stages of liver fibrosis. Shown are MRE stiffness maps in 5 patients with NAFLD. These maps depict the spatial distribution of stiffness (in kPa) within the liver (outlined in white). As shown in the color lookup table at the right, the stiffness values range from near zero (dark purple) to 8 kPa (red). The histology-determined liver fibrosis stage is shown at the top of each stiffness map, and the MRE-determined mean liver stiffness is shown at the bottom of each image. Notice that the stiffness values are greater in patients with more-advanced fibrosis.
目的:回顾性研究已经证实了一种新型的评估肝脏硬度的磁共振成像技术-二维磁共振成像(two-dimensional magnetic resonance elastography,2D-MRE)与非酒精性肝硬化(nonalcoholic fatty liver disease, NAFLD)导致的进展期肝纤维化密切相关。但仍需大量的2D-MRE诊断NAFLD准确性的前瞻性研究数据。本研究的目是前瞻性评估无创2D-MRE诊断3、4级NAFLD的准确性。
方法:本前瞻性研究采用横断面调查方法分析了117例(女性 56%)活检证实为NAFLD患者,患者检查项目包括病史、体格检查、肝穿刺活检(评估采用非酒精性脂肪肝炎临床研究组织学评分系统)、2D-MRE。随访时间从2011年到2013年。放射科医生和病理科医生分别采用盲法检测患者的影像及病理学数据。用接受者操作特征曲线(ROC曲线)评估2D-MRE对 NAFLD的诊断价值。
结果:患者平均年龄50.1±13.4岁,BMI指数32.4±5kg/m2,肝穿刺活检与2D-MRE间隔的中位时间为45天。0、1、2、3、4级肝纤维化患者人数分别43人、39人、13人、12人、10人。2D-MRE区别3-4级肝纤维化与0-2级肝纤维化的ROC曲线下面积为0.924 (P < 0.0001).阈值大于3.6KPa的灵敏性为0.86(95%的可信区间0.65-0.97),特异性为0.91(95%的可信区间0.83-0.96),阳性预测值为0.68(95%的可信区间0.48-0.84),阴性预测值为0.97(95%的可信区间0.91-0.99).
结论:2D-MRE可以准确诊断进展期肝纤维化,可以作为NAFLD进展期肝纤维化无创检查的一种方法。
原始出处
Loomba R1, Wolfson T, Ang B, Hooker J, Behling C, Peterson M, Valasek M, Lin G, Brenner D, Gamst A, Ehman R, Sirlin C.Magnetic resonance elastography predicts advanced fibrosis in patients with nonalcoholic fatty liver disease: A prospective study.Hepatology. 2014 Dec


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#MRE#
63
#进展期#
71
#AFLD#
71
#肝纤维#
70
#EPA#
70