Ann Rheum Dis:低剂量白介素-2在11种自身免疫性疾病中的临床免疫疗效
2018-11-25 xiangting MedSci原创
IL-2剂量和治疗方案可以选择性激活和扩增Tregs,并且在不同疾病和伴随治疗中是安全的。
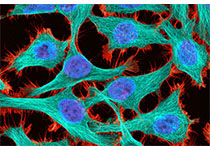
调节性T细胞(Tregs)可以预防自身免疫和控制炎症。因此,任何自身免疫性或炎性疾病都存在Treg不足。由于低剂量白介素-2(ld-IL2)能够扩增并激活Tregs,其具有巨大的治疗潜力。这是一项单一临床试验,通过交叉调查ld-IL2对11种自身免疫性疾病中任1种的疗效,来评估ld-IL2的治疗潜力并选择用于进一步临床开发的疾病。对46例轻至中度类风湿性关节炎、强直性脊柱炎、系统性红斑狼疮、银屑病、白塞病、多血管炎肉芽肿病、Takayasu病、克罗恩病、溃疡性结肠炎、自身免疫性肝炎和硬化性胆管炎患者进行了前瞻性、开放标签、I-IIa期研究。这些患者都接受了5天的ld-IL2治疗(100万IU天),然后每两周注射1次,共6个月。通过深度免疫监测和临床评估对患者进行评价。无论疾病和伴随的治疗如何,所有患者均对ld-IL2耐受良好。完全的监督和无监督免疫监测表明,所有患者存在特异性Treg扩增和活化,并不伴效应T细胞活化。观察到潜在临床疗效的提示。使用的IL-2剂量和治疗方案可以选择性激活和扩增Tregs,并且在不同疾病和伴随治疗中是安全的。这一临床疗效的初步迹象说明应该启动ld-IL2在多
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#白介素-2#
76
#Dis#
58
#临床免疫#
81
#白介素#
63
#低剂量#
46
#免疫性疾病#
53
谢谢梅斯提供这么好的信息,学到很多
63