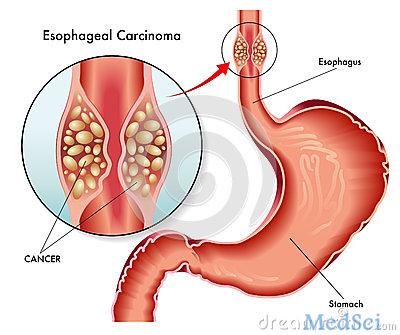
Dig Dis & Sci:内镜下切除术治疗食管鳞状细胞癌的疗效评估
2018-06-18 MedSci MedSci原创
根据日本食管学会(JES)的指南意见,食管鳞状细胞癌(ESCC)患者淋巴结(LN)转移在肌层/粘膜下深达200μm(SM1)的危险因素包括淋巴浸润(ly),静脉浸润(v),浸润模式(INF)c和SM1的存在。本项研究将探讨这些患者的长期预后以及内镜切除术(ER)后MM / SM1 ESCCs淋巴结转移的危险因素究竟是哪些。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Dis#
69
#疗效评估#
80
#内镜下切除#
81
#切除术#
60
#细胞癌#
62
学习一下
93
#食管鳞状细胞癌#
78
#内镜#
0
#食管#
59
学习谢谢分享
115