J Occup Environ Med:化学和建筑相关不耐受气道炎症性疾病的并发症分析
2017-12-29 AlexYang MedSci原创
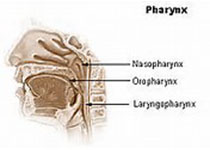
最近,有研究人员调查了慢性鼻窦炎、慢性阻塞性肺病、过敏和非过敏哮喘和过敏性鼻炎以及气道炎症症状中的化学不耐受(CI)和建筑相关的不耐受(BRI)并发症。研究人员从2个基于群体的环江健康研究调查问卷中搜集了相关数据。参与者被分成CI或者BRI组和参照组,并且还利用了二维的逻辑回归分析进行了数据分析。研究发现,案例组的疾病患病率为7.2%-40.0%,症状患病率为24.3%-68.9%,调整后的疾病让
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#炎症性疾病#
77
#并发#
60
#不耐受#
66
#OCC#
0
#iron#
65
#炎症性#
64
#Med#
55
#气道炎症#
79