世界全新术式让她避免“人工肛门”之苦!
2016-09-22 孙国根 医学论坛网
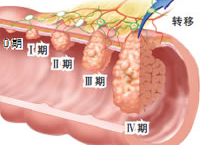
34岁的未婚外籍华人吴小姐罹患低位直肠癌,为保证根治肿瘤,传统手术往往不得不切除肛门后粪便改道,即在其腹壁上做永久性的人工肛门;为减少病人痛苦,提高病人生活质量, 复旦大学附属上海市第五人民医院普外科柯重伟教授团队克服困难,为其实施了代表目前国际直肠癌手术最新进展、最高水平的高难度的“经肛门联合经腹腔镜低位直肠癌根治术” (TaTME),既保住了病人的肛门,腹部也未留下疤痕。9月20日术后第13天
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肛门#
77
总结的很好!
120
分享一下!
105
医学越来越发达。
0
谢谢,为患者生活质量提高了
99
很不错,远期排便次数和常规DIXON术后有无差别?
96
造福此类疾患!
54
癌症的痛
62
生活质量很重要
64
继续学习
60