Clin Cancer Res:科济生物靶向GPC3的CAR-T细胞治疗晚期肝细胞癌的1期结果公布,初步取得显著疗效
2020-05-14 MedSci MedSci原创
近日,由上海交通大学医学院附属仁济医院肿瘤介入科科主任翟博教授团队与科济生物医药(上海)有限公司(“科济生物”)李宗海教授团队共同合作完成的
近日,由上海交通大学医学院附属仁济医院肿瘤介入科科主任翟博教授团队与科济生物医药(上海)有限公司(“科济生物”)李宗海教授团队共同合作完成的全球首个靶向GPC3的CAR-T细胞(CAR-GPC3)治疗晚期肝细胞癌(HCC)的I期临床研究结果在线发表于Clinical Cancer Research。
肝癌是严重威胁我国人民生命健康的重大疾病之一。流行病调查数据显示,原发性肝癌是我国第4位的常见恶性肿瘤和第3位的肿瘤致死原因,每年新发病例约46.6万。早期肝癌5年存活率50-60%,晚期肝癌中位生存期1年。
翟博认为,大多数患者确诊时已是中晚期,可能失去外科手术机会。尽管局部消融、肝动脉栓塞化疗等介入治疗为失去手术机会的肝癌患者带来了新的治愈可能,但是晚期肝癌患者复发和转移率高,必须不断研发更多高效、低毒的全身治疗手段。
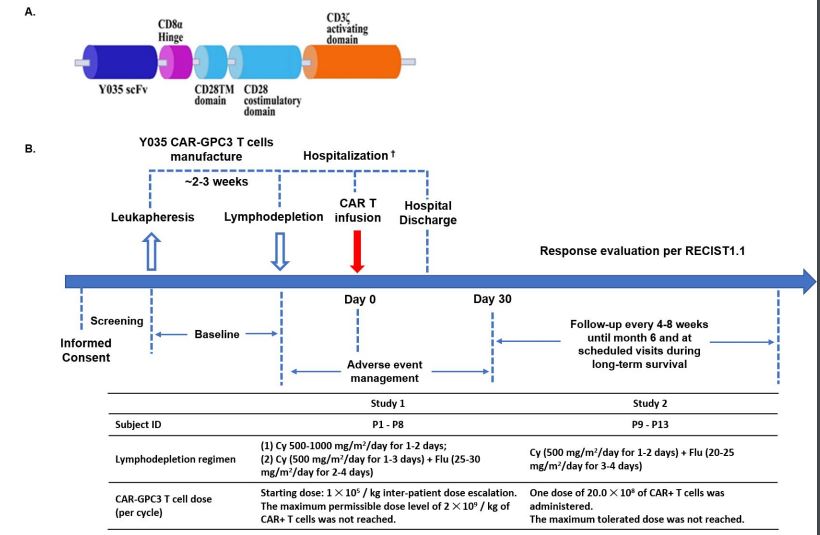
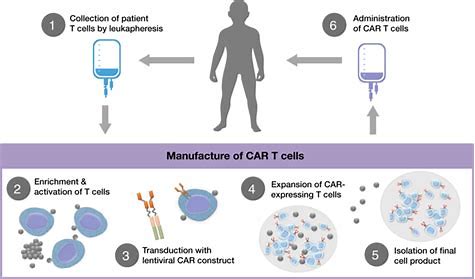
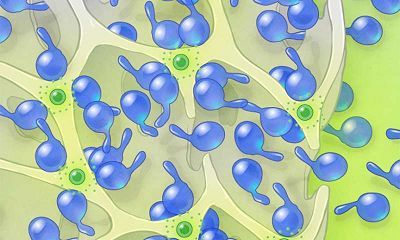
近年来CAR-T细胞治疗作为一种新兴的免疫治疗方法成为全球肿瘤治疗研究的重点和热点。CAR-T中文名叫做“嵌合抗原受体修饰的T淋巴细胞”,简单说,T淋巴细胞具有免疫活性,好似人体内的军队,是杀灭肿瘤细胞的主力军。CAR是一种分子修饰物,其装备了能特异识别肿瘤细胞的导航系统和参与免疫反应的其他分子等武器,能带着T淋巴细胞精准识别、消灭表达某种基因的肿瘤细胞,同时又不损害人体正常细胞。
2015年,由翟博教授牵头,上海科济生物公司与仁济医院合作,在全球率先开展了以GPC3为靶点的CAR-T细胞治疗晚期HCC的临床试验,治疗了13例GPC3表达阳性的晚期HCC患者,治疗的安全性和有效性均获得了令人期待的结果。接受该治疗后患者耐受性良好、安全基本可控,罕见严重毒副反应,并初步显示出较好的临床获益。
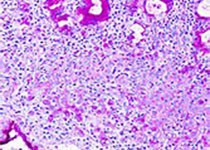
在两项前瞻性1期研究中,患有晚期GPC3 + HCC(Child-Pugh A)的成年患者在环磷酰胺和氟达拉滨诱导的淋巴清除后接受了自体CAR-GPC3 T细胞疗法。主要目的是评估治疗的安全性。
截止到2019年7月24日,共有13例患者接受了中位值为19.9×108的CAR-GPC3 T细胞。受试者整体耐受性良好,主要副作用为淋巴细胞减少,9例患者发生细胞因子释放综合征(CRS),其中8例为1/2级,预后良好。13例患者有2例获得部分缓解(PR),6个月、1年、3年生存率分别为50.3%、42.0%和10.5%,中位生存时间(OS)为278天(95%CI:48,615天)。这两例患者生存时间分别是20.5和44.2个月,其中一例疾病稳定的患者在入选时已有下腔静脉癌栓、右心房癌栓以及淋巴结转移,治疗后AFP(甲胎蛋白)长期维持正常水平且长期生存。
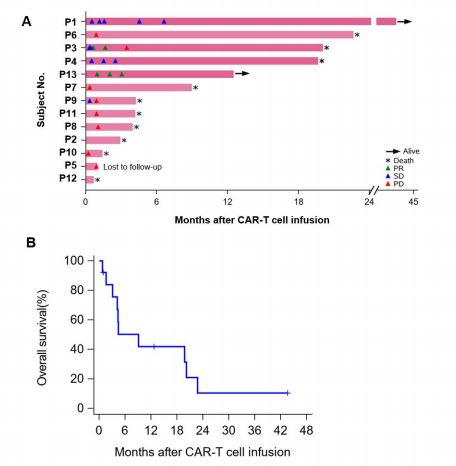
这样研究表明CAR-GPC3 T细胞疗法的初步安全性。我们观察到晚期肝癌患者CAR-GPC3 T细胞抗肿瘤活性的早期迹象。
翟博指出,该研究还有很多需要完善之处,未来要走的路还很长,但这毕竟为CAR-T细胞治疗肝细胞癌等各种实体瘤积累了宝贵经验,同时也表明CAR-T细胞的确有可能给部分肝癌患者带来长期获益。
GPC3是一种癌胚抗原,参与细胞增殖、分化、迁移和凋亡。正常组织中几乎未见表达,但在70-80%的HCC中表达。GPC3因其肿瘤特异性,被认为是极有前景的肿瘤免疫治疗靶标。
李宗海介绍,“这是全球首个靶向GPC3的CAR T细胞的临床研究,衷心感谢翟博教授团队和所有合作伙伴的贡献和支持,感谢所有患者及家属的理解和信任,没有他们的勇敢尝试,这些原创性产品是不可能推进的。衷心祝愿他们保持健康,这是新药研发的最大动力。同时,科济生物将进一步针对GPC3表达阳性的肝癌患者进行一系列探索研究。科济生物将不遗余力开发CAR-GPC3 T细胞产品,以期早日造福广大肝癌患者。”
原始出处:
Chimeric Antigen Receptor-Glypican-3 T-Cell Therapy for Advanced Hepatocellular Carcinoma: Results of Phase 1 Trials.Clin Cancer Res . 2020 May 5:clincanres.3259.2019. doi: 10.1158/1078-0432.CCR-19-3259.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#肝细胞#
0
#科济生物#
77
#CAR-#
67
#GPC3#
60
#细胞癌#
58
#结果公布#
53
#晚期肝细胞癌#
63
谢谢梅斯提供这么好的信息,学到很多
82