JAMA Oncol:术后放疗(PORT)治疗手术完全切除并完成术后辅助化疗的pIIIA-N2 NSCLC患者的疗效和安全性:III期临床研究PORT-C
2021-06-27 yd2015 MedSci原创
手术完全切除并完成术后辅助化疗的pIIIA-N2 NSCLC患者,术后放疗(PORT)并不能改善无病生存期(DFS)。
有研究发现术后放疗(PORT)似乎可以改善非小细胞肺癌(NSCLC)患者的预后。但是PORT在pIIIA-N2 NSCLC患者的作用不明确。III期临床研究PORT-C目的就是为了评估pIIIA-N2 NSCLC患者完全切除术后和辅助化疗后应用PORT的疗效和安全性。相关研究成果发表在JAMA Oncology杂志上。
研究纳入2009年1月至2017年12月期间,手术完全切除并完成术后4周期铂类为基础的辅助化疗的pIIIA-N2 NSCLC患者,共394例。随机分配至PORT组(202例)和观察组(192例)。总PORT剂量为50Gy。2019年3月至2020年12月之间进行数据分析。主要终点为无病生存期(DFS)。次要终点包括总生存期(OS)、局部无复发生存期(LRFS),无远处转移生存和毒性效应。
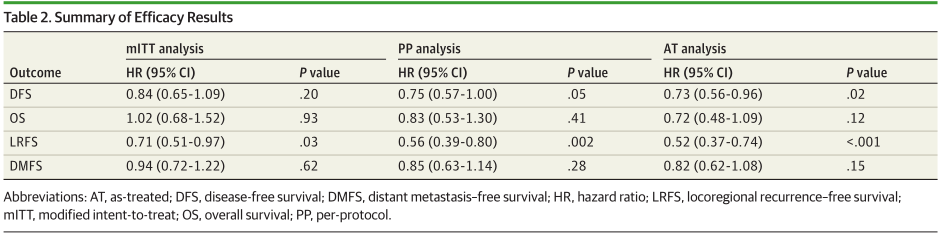
共纳入394例患者,其中364例可评估疗效,中位年龄为55岁(25 - 70)年。男性202例(55.5%),女性162例(44.5%)。中位随访时间为4 6.0个月(95%CI, 41.9-51.4),报道了230例DFS事件。两组中位DFS分别为22.1个月 (95% CI, 14.8-29.3)和18.6个月(95%CI,14.3-23.0)。3年DFS率分别为40.5%和32.7%,没有统计学差异(HR=0.84; 95% CI, 0.65-1.09; P =0 .20)。
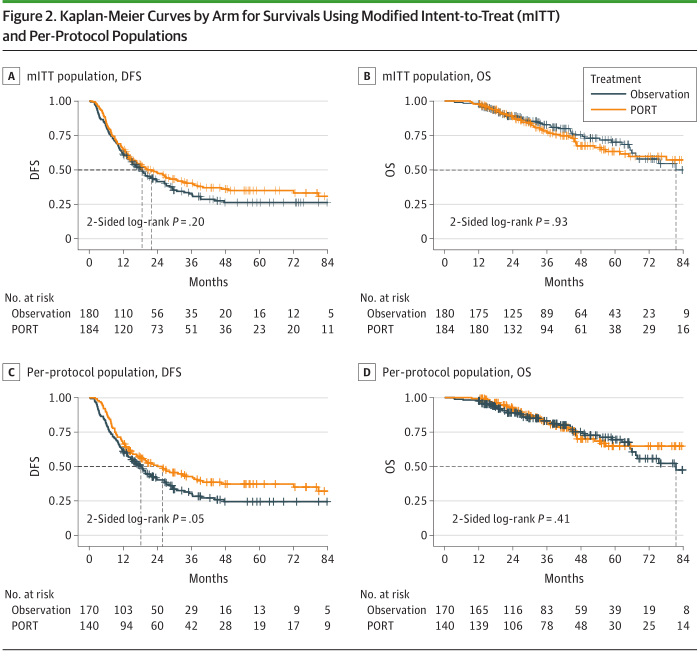
两组DFS和OS
两组中位OS分别为未达到和81.5个月(95%CI,61.6-101.4); 3年OS率分别为78.3%和82.8%, respectively (未调整HR=1.02; 95% CI, 0.68-1.52; P = 0.93; 分层HR=0.92; 95% CI, 0.61-1.39; P =0 .70)。
两组的3年LRFS率分别为66.5%和59.7%,两组间差异显著(HR=0.71;95% CI, 0.51- 0.97; P =0 .03); 3年DMFS率分别为42.0%和38.2% (HR=0.94; 95%CI,0.72 -1.22; P = 0.62)。
疗效评估
两组的3年仅局部复发率(例如,不包括同时局部复发和远处转移)分别为9.5%和18.3%(P = .04); 而两组的3年仅远处转移率(例如,不包括同时局部复发和远处转移)分别为38.4%和38.1% (P =0 .93)。
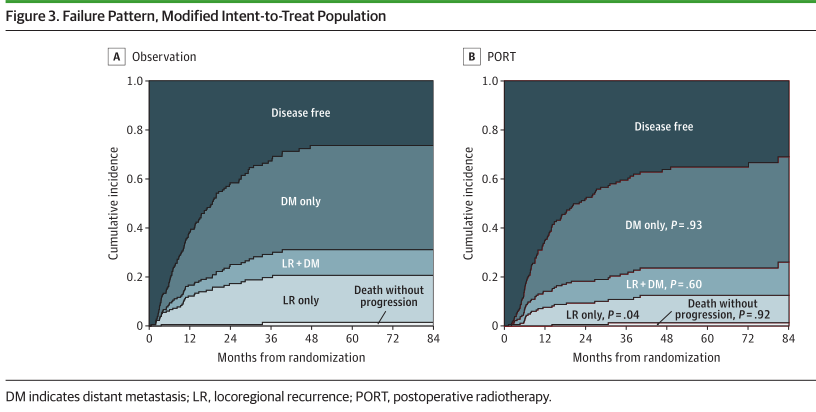
进展模式
未观察到与放射治疗相关的4级或5级不良事件(AEs)。2级及以下放射性食管炎和放射性肺炎有55例(36.6%,1级27.3%,2级9.3%),20例(13.3%;1级:8%,2级:5.3%)。仅有1例(0.7%)为3级放射性肺炎。未见3级放射性食管炎。截至最后一次随访,共有97例死亡;其中PORT组50例死亡中有47例(94.0%),观察组47例死亡中有42例(89.4%)是由于肿瘤进展引起。在8例非癌症相关死亡病例中,1例死于第二例癌症; 3例因心肺疾病; 2例因药物AEs; 1例因抑郁而自杀;1例未知原因。
综上,手术完全切除并完成术后辅助化疗的pIIIA-N2 NSCLC患者,术后放疗(PORT)并不能改善无病生存期(DFS)。
原始出处:
Zhouguang Hui;Yu Men;Chen Hu; et al. Effect of Postoperative Radiotherapy for Patients With pIIIA-N2Non–Small Cell Lung Cancer After Complete Resection and Adjuvant Chemotherapy: The Phase 3 PORT-C Randomized Clinical Trial. JAMA Oncol. Published online June 24, 2021. doi:10.1001/jamaoncol.2021.1910
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#术后放疗#
44
#I期临床#
47
#SCLC患者#
49
#疗效和安全性#
47
#II期临床研究#
57
#III#
32
#III期临床研究#
38
理学主题
50
#Oncol#
37
#III期#
39