AJOG:晚期子宫内膜癌是否有必要进行肿瘤细胞减灭术?
2021-05-18 Nebula MedSci原创
大部分晚期子宫内膜癌患者在肿瘤细胞减灭术后的残留肿瘤病灶较小(肉眼不可见或<1cm),与相对较好的无进展生存期和总生存期相关
子宫内膜癌是女性第四常见的癌症。子宫内膜癌早期即可出现异常的阴道出血/排液,约80-90%的病例在早期确诊。少见子宫内膜癌患者确诊时已是晚期,因此,目前缺乏可指导晚期子宫内膜癌的诊疗的前瞻性证据。
本研究旨在总结肿瘤细胞减灭术(PCS)治疗晚期子宫内膜癌的效果。
Albright等人采用检索词“子宫内膜癌”、“晚期”和“肿瘤细胞减灭术”检索了MEDLINE、Embase和Scopus数据库从创建到2020年9月11日期间包含≥10例接受PCS治疗的晚期子宫内膜癌患者、并有根据PCS后残留肿瘤程度报告发病率和生存结果的全英文文献。两个审稿人独立筛选研究,并由第三个审稿人审核。
共筛查了1219项研究,最终纳入了其中34项研究,包含单中心和多中心研究、跨越6-24年、各种病理类型(子宫内膜样/浆液性/透明细胞/癌肉瘤)和分期(III/IV期)。
在针对PCS后残留病灶多少的荟萃分析中,高达52.1%的病例无肉眼残留病灶 (18项研究,1329位患者),75%的病例的残留病灶低于1cm (27项研究,2343位患者)。
在IV期与III-IV期疾病的研究中,肿瘤细胞减少到上述两个阈值的比例都较低(NGRD:41.4% vs 69.8%;<1 cm:63.2% vs 82.2%),但没有明显的组织学差异。
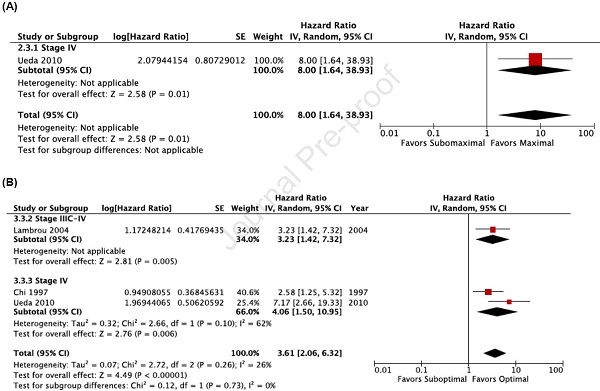
肿瘤细胞减灭程度与无进展生存期(A)和总生存期(B)的相关性
在针对报告的危险比(HR)进行分析时,与NGRD相比,任何可见残留病灶与较差的无进展生存期和总生存期相关(HR分别是2.16, 95%CI 1.45-3.21;I2=68%和2.57, 95%CI 2.13-3.10;I2=1%);与残留病灶<1cm相比,残留病灶≥1cm与较差的无进展生存期和总生存期相关(HR分别是2.55, 95%CI 1.93-3.37;I2=63%和2.62, 95%CI 2.20-3.11;I2=15%)。仅限于高质量研究的敏感性分析结果一致。
总而言之,一定比例的接受PCS治疗的晚期子宫内膜癌患者有残留的肿瘤病灶,与较差的生存预后相关;换言之,大部分患者PCS后的残留肿瘤病灶较小(肉眼不可见或<1cm),与相对较好的无进展生存期和总生存期相关。
原始出处:
Albright Benjamin B,Monuszko Karen A,Kaplan Samantha J et al. Primary cytoreductive surgery for advanced stage endometrial cancer: A systematic review and meta-analysis.[J] .Am J Obstet Gynecol, 2021, https://doi.org/10.1016/j.ajog.2021.04.254
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#晚期子宫内膜癌#
45
#肿瘤细胞减灭术#
57
#内膜#
37
#肿瘤细胞#
66
很好吧
64
学习
63
具体情况具体分析
61
学习了,谢谢
72
学习了😆
66
学习
41