Arterioscler Thromb Vasc Biol:胆结石增加民众患心脏病的风险
2016-08-19 MedSci MedSci原创
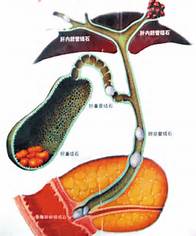
胆结石是指发生在胆囊内的结石所引起的疾病,在高收入国家较为常见,发病率为10-15%。胆结石的成因非常复杂,有些是不可更改的因素,例如:逐渐增长的年龄、女性、种族、基因和家族史;有些是后天因素,部分是可以逆转的,例如:妊娠、肥胖、低纤维、高热卡饮食结构、长时间禁食、某些药物如头孢曲松,降脂药、口服避孕药、快速体重丧失(>1.5kg/wk)、代谢综合征、特殊疾病等等。一般较小,通常没有明显表现
胆结石是指发生在胆囊内的结石所引起的疾病,在高收入国家较为常见,发病率为10-15%。胆结石的成因非常复杂,有些是不可更改的因素,例如:逐渐增长的年龄、女性、种族、基因和家族史;有些是后天因素,部分是可以逆转的,例如:妊娠、肥胖、低纤维、高热卡饮食结构、长时间禁食、某些药物如头孢曲松,降脂药、口服避孕药、快速体重丧失(>1.5kg/wk)、代谢综合征、特殊疾病等等。一般较小,通常没有明显表现,但是近年来胆结石有增大的趋势。严重者会阻塞胆管,导致患者出现严重的腹痛,即为胆绞痛。
发表在Arterioscler Thromb Vasc Biol的研究指出,胆结石是心脏病的风险因素之一。虽然看起来两种疾病看似毫无关联,一个与循环系统有关,另一个属于消化系统疾病,但二者之间有密切关联。胆结石和心脏病的风险因素非常相似,包括肥胖、糖尿病、高血压、不良的饮食习惯和高胆固醇等。然而,杜兰大学的研究人员指出,二者之间的关系不止于此。
杜兰大学流行病学Lu Qi教授和同事对超过84万名参与者进行了一项荟萃分析,其中冠心病患者超过50000名。他们研究的目的是观察冠心病和胆结石之间的关系。分析表明,胆结石病史会使民众患冠心病的风险增加23%。研究结果表明,胆源性疾病患者应密切监测自己的心脏功能,同时调节生活方式和饮食等预防心脏病的发生,预防胆石病也有利于心脏健康。
在第二个研究中,研究人员对26万多名参与者进行了探究,Lu Qi博士发现即便一些表现正常的胆石病患者(体重、血压、血糖正常)患心脏病的风险也高于未患胆石病的患者。胆石病是导致民众患心脏病的独立风险因素。这一结果与既往研究结果相似。
第一次大规模研究显示,即便没有普遍风险因素的存在,胆石病也是导致民众出现心脏病的独立风险因素。但荟萃分析不能确定这种关系的真正原因,有研究人员认为,胆结石改变胆汁酸的分泌,这与心血管疾病的出现有关。而胆汁酸的分泌与肠道微生物群有关,因此研究人员致力于研究三者之间的关系。
原始出处:
[1] Gallstones raise the risk of heart disease by a fifth. MNT.2016 August 19.
[2] Lu Qi et al. Gallstones and risk of coronary heart disease: Prospective Analysis of 270 000 men and women From 3 US cohorts and meta-analysis. Arteriosclerosis, Thrombosis and Vascular Biology, doi: 10.1161/ATVBAHA.116.307507, published online 18 August 2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Bio#
35
#ASC#
37
#Biol#
35
文章很好值得关注
67
很好学习。
75
学习了,好
68
继续关注
77
这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
62
这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
32
阅读了。
33