Lancet Oncol:双抗Mosunetuzumab治疗复发或难治性滤泡性淋巴瘤的疗效
2022-07-18 MedSci原创 MedSci原创
固定疗程的Mosunetuzumab可为复发或难治性滤泡性淋巴瘤患者提供高缓解率
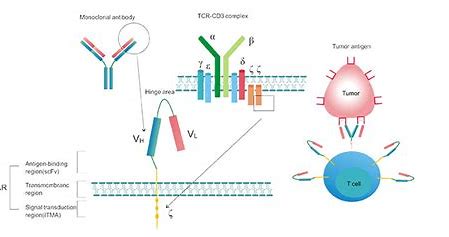
Mosunetuzumab 是一种 CD20×CD3 双特异性单克隆抗体,可重定向 T 细胞以消除恶性 B 细胞。在一项1期研究中,Mosunetuzumab 在复发或难治性B细胞淋巴瘤中的耐受性良好,而且表现出了治疗活性。
因此,该研究旨在评估固定疗程的 Mosunetuzumab 在既往至少接受过两次治疗的复发或难治性滤泡性淋巴瘤中的抗肿瘤活性和安全性。
这是一项国际性、多中心、单组的2期研究,招募了年满18岁、组织学明确诊断的、ECOG表现状态0-1分的滤泡性淋巴瘤(1-3a级)患者。予以Mosunetuzumab治疗(21天为一疗程)。获得完全缓解的患者接受8个疗程的治疗,获得部分缓解或病情稳定的患者持续治疗最多17个疗程。主要终点是完全缓解率,并与接受pan I类PI3K抑制剂Copanlisib治疗的类似患者群体中14%的完全缓解率进行比较。
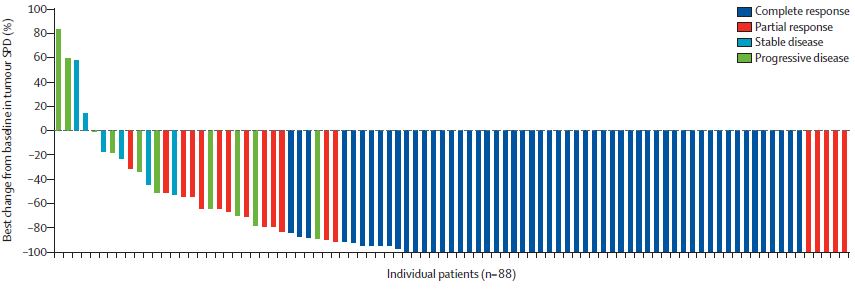
每位患者的最佳缓解情况
2019年5月2日-2020年9月25日,共招募了90位患者。截止2021年8月27日,中位随访了18.3个月。54位(60.0%)患者获得了完全缓解。观察到的完全缓解率显著高于Copanlisib治疗的历史对照完全缓解率(14%,p<0.0001),因此,实现了主要研究终点。
受试患者的无进展生存率和缓解持续时间
细胞因子释放综合征是最常见的不良反应(44%),主要是1级(26%)和2级(17%)的,主要发生在第1个疗程。最常见的3-4级不良反应有中性粒细胞减少或中性粒细胞计数减少(27%)、低磷血症(17%)、高血糖(8%)和贫血(8%)。42位(47%)患者经历了严重不良反应。无治疗相关5级(致死性)不良事件发生。
综上,固定疗程的 Mosunetuzumab 在复发或难治性滤泡性淋巴瘤患者中具有良好的安全性,并可诱导高完全缓解率,为治疗失败两次的患者提供了潜在选择。
原始出处:
Lihua E Budde, et al. Safety and efficacy of mosunetuzumab, a bispecific antibody, in patients with relapsed or refractory follicular lymphoma: a single-arm, multicentre, phase 2 study. The Lancet Oncology. July 05, 2022. https://doi.org/10.1016/S1470-2045(22)00335-7
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
112
#NET#
114
#Oncol#
95
#mAb#
72
#滤泡性淋巴瘤#
92
#双抗#
63
#难治性#
73
认真学习~
76
lancet上果然牛,感谢梅斯更新及时
68