罕见!结肠息肉切除术后竟发生了这种并发症
2019-04-25 王胤 陆兴俊 医学界消化肝病频道
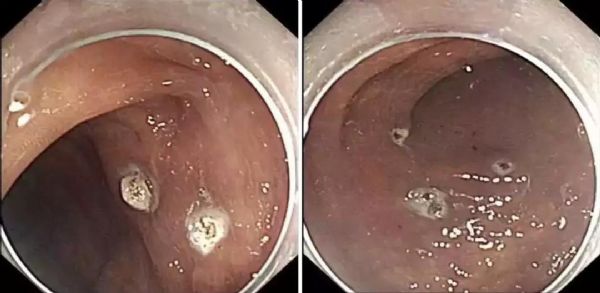
患者,女,56岁,因“发现结肠息肉3天”入院,患者3天前因腹胀、解大便困难前往我院门诊就诊。患者无反酸烧心,无恶心呕吐,无腹痛、腹泻,自诉解大便困难,平均3天一次,为黄色成型大便,偶有运用“导泻药物”,具体不详。予以肠镜检查示:距离肛门口40cm以下见大小为0.2-0.5cm的息肉,诊断为:结直肠多发息肉,结肠黑病变。现患者为进一步内镜下息肉切除术,入住我院消化内科。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#切除术#
50
#并发#
64
学习了
80
#罕见#
57
#息肉切除术#
75
学习了
87