汇总!关于慢性肾病,你必须了解的研究进展!
2017-03-14 MedSci MedSci原创
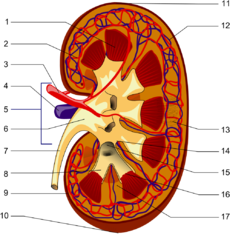
肾病,人体脏腑之间,内环境与外环境之间均保持着动态平衡。内外界多种致病因素如果破坏了人体的平衡,导致脏腑气血功能失调,病及于肾,则引起肾脏疾病的产生。致肾脏疾病的病因多种多样,如六淫、七情、饮食、劳逸、房劳、药毒、意外伤害等多种内外因素均可致病。并且,在疾病的发生、演变过程,病因和其病理产物常互相作用,互为因果。本文梅斯小编整理了近期慢性肾病相关研究进展,与大家分享。【1】Nat Rev Ne
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#研究进展#
47
感谢分享一下!
85
谢谢分享,学习了
104
学习了,很有用处不错
82
学习了谢谢分享
90
学习了,谢谢
74
学习了谢谢分享
61
学习了不错
47
谢谢分享
73
很好的学习资料,谢谢了。
62